|
|||||||||||||
AbstractWegener's Granulomatosis(WG); rare primary upper respiratory tract, lower respiratory tract and kidneys that are characterized by systemic vasculitis. Limited involvement of the disease is non-renal vasculitis and good, slow prognosis form. Approximately half of the patients are otitis media with effusion, chronic otitis media and sensorineural hearing loss, external otitis can accompany the disease, such as involvement in otologic. In this article we only progressive otologic involvement, c-ANCA positivity identified; histopathological diagnosis of cyclophosphamide and methylprednisolone in the treatment of placed with a rare case of the WG provided remission, accompanied by limited literature are discussed.IntroductionWegener granulomatosis(WG) is a necrotizing granulomatous vasculitis involving especially the small and medium sized vessels. Its prevalence is 3/100,000. This disease has a classical histologic triad composed of necrotizing granulomatous inflammation in the airway, systemic vasculitis involving mainly the small vessels, and focal glomerulonephritis. While the main prognostic factor is usually renal involvement, systemic disease may present with upper respiratory tract involvement only [1]. Two main variants of WG have been defined: generalized and limited. Limited WG is the variant with a good prognosis and slow progression with no renal involvement or systemic vasculitis. This variant was defined by Carrington and Liebow in 1966 [2]. Otologic involvement is seen in 30% of the patients. The most commonly seen manifestations of otologic involvement are otitis media with effusion, sensorineural hearing loss, chronic otitis media, and otitis externa [3]. In this article we report a rare case of limited WG which manifested as bilateral chronic otitis media with no renal or pulmonary involvement and was diagnosed histopathologically and by c-ANCA positivity. Case ReportA 30-year-old female was referred to the outpatient clinic with a right-sided otorrhea, otalgia, vertigo and hearing loss with duration of 2 weeks. The detailed history revealed that the complaints had first appeared 3 months ago after a viral upper respiratory tract infection.There had been an improvement but no complete resolution of her complaints after treatment consisting of systemic and topical antibiotics and topical steroid ear drops given by another otolaryngologist. On physical examination, there was a subtotal perforation on the right tympanic membrane, with purulent discharge and keratin debris (Figure 1a).
Direct and endoscopic examination of the nasal cavity, nasopharynx, oropharynx and larynx was normal except some findings suggesting a mild upper respiratory infection. The discharge of the ear resolved after treatment. The patient referred after 4 weeks of the initial examination with a complaint of left-sided otorrhea and otalgia; on examination, there was a central perforation on the left tympanic membrane with a purulent discharge (Figure 1b).
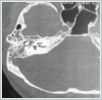
Bilateral facial nerve functions were intact and the fistula test was negative. The patient was hospitalized. The high resolution temporal computerized tomography imaging demonstrated infiltrative soft tissue density in the right mastoid and middle ear cavities consistent with otomastoiditis (Figure 2a).
The posteroanterior chest X-ray was completely normal. On pure-tone audiometry, there was a conductive hearing loss, with average air/bone thresholds of 48/12 dB HL on the right and 28/10 dB HL on the left ear (Figures 2b and 2c).
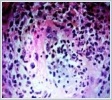
On laboratory workup, there was leukocytosis (WBC 12,5 103/ml). The erythrocyte sedimentation rate and CRP were high at 37 mm/hr and 56 mg/L, respectively. Brucella agglutination and p-ANCA were negative. However, c-ANCA was positive at 1/10th dilution, and tissue biopsy was obtained from the external and middle ear mucosa under local anesthesia. Histopathologic examination of the specimen demonstrated vasculitis and granulomatous inflammation (Figure 1c). The patient was then referred to the rheumatologist with a probable diagnosis of WG.
Since there was no renal or respiratory involvement, the case was diagnosed as limited WG. Oral cyclophosphamide (100 mg/kg daily) plus IV methylprednisolone (1 mg/kg daily) was started. While metylprednisolone has been tapered off at the end of 3 months, the patient is still receiving cyclophosphamide. Now the disease is on remission and right tympanoplasty has been planned. DiscussionThe classical diagnostic finding in Wegener’s granulomatosis is necrotizing vasculitis involving the upper and lower respiratory tract and the kidneys. Both genders are equally affected. Although the etiology remains unknown, it is thought to develop as a hypersensitivity response against a number of inhaled antigens [4]. In the systemic variant of this disease which is more commonly seen (85-90% of all cases), otorhinolaryngologic manifestations can be seen as ulceration and destruction in the nasal cavity and paranasal sinuses (and resultant mucosal hemorrhage), saddle nose deformity, sinusitis findings, otitis media with effusion, hearing loss, and tracheal stenosis. Yamazaki et al. reported thick ear drums with pulsatile serous intratympanic effusion in their cases, identified poor speech discrimination and hearing levels. They thought that vasculitis of stria vascularis which generates endocochlear potential might cause a reversible cochlear dysfunctions [4] . Even there were the otologic involvement in our patient. Although Hoffmann et al. reported the rate of nasal mucosal vasculitis and chronic vasculitis as 10% and 14% respectively [5], our case exhibited no nasal or sinüs involvement. Savage et al. [6] reported 60-80% rate of respiratory symptoms and 50% rate of signs such as pulmonary infiltration, nodular involvement and cavitary lesions, none of which were detected in the currently reported case. Renal involvement is encountered in 70-80% of cases of the systemic variant, with subsequent renal failure if left untreated [7]. Apart from renal involvement, other manifestations that might be detected are splenic infarcts, gastrointestinal hemorrhage, orbital involvement, and ischaemic coronary disease. Our case did not exhibit renal involvement. The limited variant of the disease in which there is no systemic vasculitis or renal involvement, which is mainly seen in females, may progress to systemic form with time [2]. Otologic involvement may contribute to 30-40% of the cases. Otitis media with effusion resulting from granulation in the Eustachian tube, nasal cavity and nasopharynx, hearing loss of sensorineural or conductive type, chronic otitis media due to inflammation in the mastoid cells or the middle ear mucosa (as seen in our case), and facial paralysis (10%) resulting from otomastoiditis are among the possible otologic manifestations. Tagaki et al. detected otologic involvement in 60% of the cases in their retrospective study, 60% of which being chronic otitis media, 27% otitis media with effusion, and 13% hearing loss. They also reported nasal cavity and paranasal sinus involvement in 93% of the patients with otologic manifestations [8]. In addition to the clinical findings, appearance of sclerotic sinus wall and bony destruction with new bone formation in computerized tomography(CT) and magnetic resonance imaging(MRI) are the characteristic diagnostic findings of WG in patients with no prior nasal or sinus surgery. These radiologic changes are helpful in patients in whom c-ANCA is negative and the clinical findings are obscure [9]. There were findings suggestive of otomastoiditis in the axial temporal CT imaging of the currently reported case.(figure 4). The four diagnostic criteria defined by American Rheumatology Association for WG are as follows:
Satisfaction of 2 or more of these criteria is needed for diagnosis of WG [10]. A positive ANCA (antineutrophil cytoplasmic antibody) is an important laboratory finding for this disease. c-ANCA has an important role in the follow-up of response to treatment, remission and relapse. In the reported case, the diagnosis of limited WG was established by the satisfaction of the 1st and 4th criteria, combined with a test result positive for c-ANCA. The main treatment regime in WG is the combination of cytostatic agents and corticosteroids. Cyclophosphamide plus corticosteroid is the most commonly used combination. Maintenance treatment is recommended for 1 year after remission. Methotrexate may be an alternative in patients in whom cyclophosphamide cannot be used. Rate of clinical cure is high. The success rates can be as high as 90% in patients diagnosed and treated at an early stage of the disease [11]. 80% of the patients who are left untreated may die. Conclusion Although systemic necrotizing vasculitis is a usual observation in the course of WG, this disease is among the bunch of clinical entities which should be considered in the differential diagnosis in cases of chronic otitis media progressing despite standard medical treatment. Since WG may affect any organ system in the body, the diagnosis of cases with limited types and atypical presentations is possible with only a high degree of suspicion. Early diagnosis and prompt treatment are of paramount importance for the control of this disease at its early stages. References
|
|||||||||||||
| Keywords : Sınırlı wegener granülomatozis , Sistemik vaskülit , Akciğer/böbrek tutulumu , Otolojik görünüm , Biyopsi , Siklofosfamid , Prednizolo | |||||||||||||
|