|
|||||||
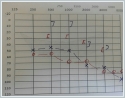
AbstractGranulomatosis polyangiitis (GPA) that usually progresses through involvement of upper and lower respiratory tracts and renal system has various otological findings; however presence of peripheral facial paralysis together with otological involvement is extremely rare. A GPA case that 42-year-old female patient with bilateral serous otitis media, left facial paralysis and left parotitis is presented in this report. Early diagnosis of GPA is important for prevention of disease progression, irreversible phase and redundant surgical intervention.IntroductionGranulomatosis with polyangiitis (GPA), also known as Wegener's granulomatosis (WG), is a systemic disorder with unknown etiology that involves both granulomatosis and polyangiitis. It is a type of anti-neutrophile cytoplasmic antibodies (ANCA)-related vasculitis that involves small and medium sized vessels. It primarily affects upper and lower respiratory tracts and kidney [1] . Although otological involvement in GPA could be observed in 35-40% of cases, finding otological symptoms is rare when the disease is already recognized [2,3] . The most common forms of ear involvement are sensorineural hearing loss, serous otitis media (SOM), chronic otitis media and otitis externa [4] . C-ANCA is rather specific to active phase GPA[5] . Biopsy histopathology is usually not specific. The difficulty in early diagnosis causes a delay in treatment and causes the disease to enter the irreversible phase [6]. This case study is presented to state the ground of c-ANCA in early diagnosis of GPA cases that start with bilateral serous otitis media (SOM) and unilateral parotitis and facial paralysis and the importance of starting a treatment before the classical GPA manifestation settles. Case ReportAfter informed consent was taken from the patient this report prepared. 42-year-old female patient consulted our otolaryngology clinic with complaints of pain, sensitivity and swelling on the left part of the face, pain and fullness in both ears and hearing loss that continued for seven months. Medical history of the patient revealed no previous disease story. Her physical examination showed bilateral glu-ear. No anomalies were shown in endoscopic larynx and nasopharynx examinations. A pure-tone audiogram was performed by using an AC40 Diagnostic Audiometer (Interacoustic Company, Denmark) and revealed moderate-severe hearing loss (70/30 dB) in the right ear and moderate mixed-type hearing loss (50/15 dB ) in the left ear (Figure 1).
Tympanometry was flat (Type B) on both ears. A computed tomography (CT) of the temporal bone showed thickening of mucosa in the middle ear, petrous apex and mastoid cavities without bone erosion . Magnetic resonance imaging (MRI) of the temporal bone showed bilateral inflammatory signal at the mastoid cells, middle ear cavity and petrous apex. Bilateral ventilation tubes were applied to the patient but one day later they were removed from tympanic membrane through pulsatile ear discharge and patient received a bilateral T-tube ventilation silicon tube (Medtronic Xomed, Jacksonville, FL, USA) application. The patient’s complaints declined and there was a decrease in air-bone gap. The hearing levels was 53/33 dB in the right and 45/27 dB in the left ear at pure-tone audiometry after 1 month. But patient consulted our clinic again after 4 months with complaints of sensitivity in left parotis region and pain in the left ear. ENT examination revealed serous drainage from T-tube on the left tympanic membrane. MRI of parotis region showed right parotitis in the gland (Figure 2).
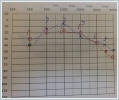
Ultrasonography and fine needle aspiration biopsy (FNAB) from parotis showed non-specific inflammatory tissue. During the course of antibiotherapy for parotitis, the patient developed a left facial paralysis (stage II-III of House-Brackmann). The patient did not have any systemic findings and her posteroanterior chest X-ray was normal. Serology using enzyme-linked immunosorbent assay (ELISA) for c-ANCA tested positive with a titer of 37.4IU/ml. Rheumatoid factor (RF), antinuclear antibody (ANA), anti-double stranded DNA (Anti-DS DNA), anti-cyclic citrullinated peptide (Anti CCP), anti-smith antibody (Anti Sm) were negative. Serology for herpes simplex and epstein-barr virus antibody, tuberculin skin test was negative. C-reactive protein (CRP) was 18 mg/dl and erythrocyte sedimentation rate (ESR) was 35 mm/hour. While these analyses were being done, the patient started to have pretibial petechia. The diagnosis of GPA was made based on these findings. Treatment with oral prednisolone (Deltacortril (R); Pfizer) (1 mg/kg/day) and oral methotrexate (Methotrexate Ebewe (R); Sandoz) (25mg/week) were initiated. One month later, the hearing loss and the facial palsy had reverted and ESR was 28 mm/hour. On the sixth month of the treatment, the patient did not have any complaints and was maintained on metotrexate (12.5mg/week) and prednisolone (16mg/day). The audiogram showed normal pure-tone average levels in the right (18/14dB) and left ear (15/2 dB). But a residual bilateral symmetrical sensorineural hearing loss on high tones (Figure 3).
DiscussionGranulomatosis polyangiitis is a multi-systemic disease characterized by granulomatous vasculitis in upper and lower respiratory tracts and as necrotizing glomerulonephritis in kidneys. It is common between ages 15-75, especially around the age of 40 and its incidence is the same for males and females[1]. Observation of peripheral facial paralysis together with otological involvement in GPA is extremely rare [2] . Fauci et al. reported that the primary complaint of 6% of all patients is hearing loss [7] . Otological involvement in GPA is categorized under 5 groups [2,6,8,9] : 1) Serous otitis media arises as a consequence of Eustachian tube obstruction and nasopharynx involvement and usually decreases with ventilation tube application (90%). 2) Chronic otitis media emerges based on primary involvement of middle ear and mastoid cavity (24%). 3) Sensorineural hearing loss is observed in 43% of the patients that have cochlear involvement and immune deposits accumulation in the cochlea. Chronic otitis media and sensorineural hearing loss do not respond to antibiotherapy. The symptoms can regress with early delivery of glucocorticoid and cyclophosphamide treatment. 4) Presence of vertigo can be explained by accumulation of immune complex in vestibular compartment. 5) Facial nerve paralysis is observed in 8-10% of the patients. It usually arises causes of dehiscence in middle ear, pressure on fallopian channel and vasculitis in facial microvascular structures. Several case studies reported that the findings get worse after myringotomy and facial paralysis occurs after mastoidectomy [3] . It could not be differentiated if the facial paralysis occurs as a result of the surgical operation or the natural course of the disease. However it is very critical to decide upon surgery in the active stage of the disease. Salivary gland enlargement is rare in GPA; usually parotis and submandibular glands are affected. Up to day, about 10 cases have been reported with parotis gland involvement [10]. Salivary gland involvement can be an early sign of GPA and can be an important sign for early diagnosis of the disease. Initiation of treatment in the early period could prevent irreversible organ damage [10]. Early diagnosis is possible with ESR measurement and serological c-ANCA analysis. Observation of granuloma in the histopathological examination of nasal mucosal biopsy would support granulomatosis polyangiitis diagnosis. It is important to start immune-suppressive treatment in the early stage to prevent redundant and potentially dangerous middle ear surgery. ESR measurement and c-ANCA levels are critical markers for the follow-up of patient, investigation of the response to treatment and re-activation of the condition in the early period [2]. In our case, the addition of facial paralysis and pretibial petechia to the unresolved serous otitis media accompanied by mixed type hearing loss aroused the suspicion of systemic disorder. CT of the thorax and abdomen did not show any pathological findings. The patient was followed up during her medical treatment and the patient did not bother any GPA symptom. Early diagnosis of GPA is critical for prevention of progression and irreversible phase of the disease and also for the prevention of a redundant surgical operation. There is not any financial disclosure statement and conflict of interest regarding the submission and publication of the manuscript and its potential implications. References
Presented atPoster presentation at the 37th National ENT & Head & Neck Surgery Congress (28 Oct- 1 Nov 2015 Antalya-Turkey) |
|||||||
| Keywords : Granulamatozis polianjitis , Seröz otit , Fasiyal paralizi , Parotitis | |||||||
|