|
|||||
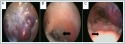
AbstractHemangiomas are benign vascular tumors which can arising from skin, mucosal surfaces and deep body parts such as muscles, bones and secretory glands. In the head and neck region they usually localized in the oropharynx and rarely in the nasopharynx. A 21-year-old female patient was consulted with nasal obstruction and frequent epistaxis. According to endoscopic examination and magnetic resonance imaging study a giant hemangioma was detected that originating from nasopharynx and extending to hypopharyx. Absolute alcohol(ethanol) was used as sclerosing agent in the treatment because of the size and localization of the tumor and the lesion regressed after treatment. 18 months follow up examination of the patient revealed no sign of recurrence.IntroductionHemangiomas are benign vascular tumors which can be detected in skin, mucosal surfaces and deep body parts such as muscles, bones and glands. They usually occur in infants and children and the incidence is reported 4-10% in Caucasian neonates with male to female ratio of 1:5 [1]. Head and neck is the most frequent site (60% of the cases) [2], and hemangiomas of the head and neck usually seen in the oropharynx and can rarely occur in the nasopharynx [3]. In this paper we report a case of giant hemangioma presenting with nasal obstruction and epistaxis, which involved nasopharynx and hypopharynx in an adult patient. Case ReportWritten informed consent was obtained from from the patient for this case report. A 21-year-old female patient was referred our clinic for 6 months history of nasal obstruction and epistaxis. Her medical condition was good. Physical examination of the patient revealed a purple lesion on the left tonsillar region at oral cavity. Anterior rhinoscopy was normal but a purple bulky tumor was seen in the nasopharyngeal region by flexible endoscopy. The mass was originating from the left lateral wall of nasopharynx and was extending inferiorly to the oropharynx and down to the level of hypopharynx. The mass was not homogenously involving the mucosa and there were normal areas at affected region. Vocal cord movements were normal. (Figure 1)
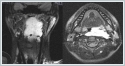
T2 weighted magnetic resonance imaging (MRI) in coronal and axial plane revealed a huge mass that resembled hemangioma in the left tonsil and pharynx with multiple ectatic vascular structures and soft tissue swelling. (Figure 2)
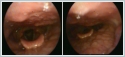
With the diagnosis of hemangioma, sclerotherapy was planned. Tracheotomy was performed under general anesthesia before sclerotherapy for preventive means due to the size and close proximity of the lesion to the airway. Local sclerotherapy was performed under sedation-analgesia. We used absolute alcohol (%100 dehydrated ethanol) as sclerosing agent. Ethanol was injected into the hemangioma with the direct puncture of the lesion with the needle. During the procedure angiography guidence showed contrast stagnation within the lesion and lack of fast venous drainage. In this way we injected agent only into the hemangioma and avoided introduction of ethanol into the systemic circulation. One month after the intervention the lesion regressed significantly and the patient was decanulated. 18 months follow up examination of the patient revealed no sign of recurrence and the patient is still symptom free. (Figure 3)
DiscussionHemangiomas are the most common vascular lesions of infancy and they usually affect head and neck region. Watson and McCarthy reported 1363 lesions of which 56% of all hemangiomas were seen in the head and neck region and 85% of lesions were seen in newborns and first year infants [4]. They rarely occur in adults. For adults, benign tumors of the nasopharynx such as juvenile angiofibroma, hemangioma, hemangiomapericytoma should be considered for differential diagnosis. But nasopharyngeal hemangiomas are rare [5]. We reported a giant hemangioma that affected nasopharynx, oropharynx and hypopharynx. There are three stages of a hemangioma which appear at infancy. The proliferating phase (0-1 year of age), the involution phase (1-5 years of age), and involuted phase (>5 years of age) [1]. Unlike infantile hemangiomas, adult lesions enlarge with age and do not involute spontaneously [1]. They usually affect supraglottic or glottic region. Adult hemangiomas are more common in males than females, which is another difference from infantile hemangiomas [6]. Our patient was female but lesion was located in a rare region, at pharyx. Symptoms of the hemangioma vary according to the site of the lesion. Stridor, hoarseness, nasal obstruction, epistaxis, bleeding, ulceration, dysphonia can be seen. Also life-threatening complications like coagulapathies (Kasabach-Merritt syndrome), airway obstruction and heart diseases (congestive heart failure) can occur [5,6]. Our patient presented with nasal obstruction and frequent epistaxis. Most hemangiomas require no intervention. If there is no symptom only periodic observation is enough. In the symptomatic cases, treatment modality varies according to location and size of the lesion, and age of the patient. Treatment options are surgical intervention, medical therapy such as local and systemic steroids, propranolol, sclerosing agents, cryotherapy, laser therapy and radiation therapy [1]. Surgical excision is the most effective therapy but in some cases total excision is not possible due to size and location. Recent studies report that steroids are the first option in medical treatment but especially systemic steroids have important side effects. Sclerotherapy with liquid denaturing agents has been an alternative treatment modality to surgical excision of hemangiomas [7]. Sclerosing agents cause denaturation of tissue proteins, endothelial damage and thrombosis of the vessels, which lead the fibrosis, arrest growth and promote regresion of hemangioma. Sodium morrhuate, sodium tetra dacylsuphate, bleomycin, sodium psylliate and ethanol are commonly used sclerosing agents in treatment of hemangiomas [8]. Ethanol is a popular choice because of its high potency, avaliability and ease of administration. Crawford at al. retrospectively reviewed 19 patients who had musculoskeletal hemangiomas. They used absolute ethanol (%100 dehydrated alcohol) as sclerosan agent to determine whether ethanol sclerotherapy reduces pain and lesion size. They concluded that sclerotherapy caused pain relief in 15 of 19 patients, so alcohol sclerotherapy was an reasonable option for initially avoiding surgical excision [9]. Seruga reported a case of cavernous hemangioma of the tongue which was treated by the direct puncture of hemangioma and sclerotherapy with ethanol. Control MRI examinations revealed only a small remnant of the tumour. There was no larger relapse after 1 year [10]. Potential complications of sclerotherapy include skin and mucosal injury, infection, nerve injury and airway problems [11]. In our case, because of the localization of the lesion we performed tracheotomy before the sclerosing agent injection. Direct injection of ethanol into hemangioma has been defined as an alternative treatment modality to surgery. Ethanol sclerotherapy offers satisfying results with easier implementation. Also direct injection of a sclerosing agent into the lesion is a better way to provide devascularization. These agents should be injected slowly to reach the maximum level at vascular bed [12]. For head and neck region, especially oversized and deep localized lesions, alcohol sclerotherapy is an effective method. References
Presented atThe manuscript presented as a poster in 37th Turkish National Congress of Otorhinolaryngology Head and Neck Surgery, 2015 October 28-November 1th, Antalya, Turkey. |
|||||
| Keywords : Hemanjiom , farenks , Skleroterapi , Saf etanol | |||||
|