|
|||||||||||||||||||
AbstractRamsay-Hunt Syndrome (RHS) is an infectious cranial neuropathy due to reactivation of varicella zoster virus in the geniculate ganglion. In this case report, we present 2 cases of RHS with unilateral facial palsy, herpetic vesicles on the auricle and multiple cranial nerve involvement treated with intravenous and oral corticosteroids, antiviral agents and antibiotics. Early diagnosis and prompt treatment, as well as accompanying comorbidities are the primary factors associated with the prognosis of RHS.IntroductionRamsay Hunt syndrome (RHS) is caused by reactivation of varicella zoster infection in the geniculate ganglion. Among cases of peripheral facial palsy, 12% are RHS. The most common symptoms of RHS are ipsilateral facial palsy, otalgia, and vesicular exanthema. Vestibulocochlear nerve involvement is also common and patients can have sensorineural hearing loss. Multineuropathy involving other cranial nerves (V,VIII-XII) is rare and such symptoms as trigeminal neuralgia, loss of gag reflex, dysphagia, hoarseness, vocal cord palsy, and tongue deviation can be seen. Herein we report 2 patients with RHS and multiple cranial nerve involvement. Case ReportPatient 1 A 33-year-old female presented with unilateral facial palsy, ipsilateral otalgia, and herpetic vesicles on the auricle. Otalgia began 1 week prior to presentation at another institution. She was examined at an emergency unit and given oral antibiotherapy, but 3 days later she had hoarseness. Left-sided facial palsy appeared 2 days after the onset of hoarseness, and she was referred to our clinic. Physical examination showed vesicular eruptions with crusts on the left auricle and bullous lesion in external ear canal (Fig 1A), left-sided facial palsy, loss of gag reflex, tongue deviation (Fig 1B), aphthous lesions, erythema and edema on the left arytenoid and left vocal cord palsy (Fig 2A).
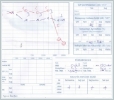
The degree of facial palsy was House-Brackmann (HB) grade 5 and audiogram showed left sensorineural hearing loss (Fig 2B).
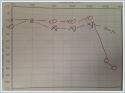
Vestibular function test was normal (Fig 3A).Cranial MRI showed no signs of disease and immunodeficiency was not detected.
Initially, IV pulse methylprednisolone with proton pump inhibitor 250 mg was given for once and treatment continued with IV acyclovir 10 mg/kg/day and oral prednisolone 1 mg/kg/day for 10 days. Two weeks post treatment she had residual HB grade 2 facial palsy (Fig 3B) and left vocal cord paresis.
Otolaryngological examination 1 month post treatment showed HB grade 1 facial palsy (Fig 4A), normal vocal cord functions (Fig 4B) and audiologic evaluation showed less severe sensorineural hearing loss (Fig 5).
A 62-year old male presented with left-sided facial palsy, herpetic vesicles on the left auricle, left-sided sensorineural hearing loss and vertigo that started 5 days after the onset of left otalgia and headache. The clinical manifestations developed gradually over few days. Hoarseness and aspiration developed 2 days after hospitalization. Physical examination showed lack of gag reflex, left vocal cord paralysis, and tongue deviation. The degree of facial palsy was HB 5 and audiogram showed left sensorineural hearing loss. Brain MRI revealed no sign of any intracranial pathology. The patient also had chronic renal failure, hypertensive heart disease, and coronary artery disease, which necessitated stenting 2 years earlier. Due to severe aspiration the patient was intubated via nasogastric tube. Methicillin-resistant staphylococcus aureus (MRSA) was cultured from deep tracheal aspiration material. Teicoplanin 10 mg/kg/day, IV acyclovir 10 mg/kg/day and oral methylprednisolone 1 mg/kg/day was initiated. Due to lack of response to teicoplanin after 1 week, antibiotherapy was switched to piperacillin tazobactam. The patient’s general health status gradually deteriorated, and after development of hypotension and hypothermia he was transferred to the intensive care unit (ICU). On day 3 in the ICU the patient had respiratory arrest followed by cardiac arrest. Following 45 min of CPR there was no response and the patient’s status was accepted as exitus. Written informed consent was obtained from the participants of this study. DiscussionAfter primary varicella infection, varicella zoster virus persists on cranial and spinal nerve ganglions. Reactivation of the virus in the geniculate ganglion and sensorial nerves of the ear causes RHS. RHS—first described by Hunt in 1907—is characterized by facial palsy, herpes zoster oticus, and sensorineural hearing loss [1]. The incidence of RHS is 5-10/100,000 and it accounts for nearly 12% of all facial palsies. Rare cases of RHS with other cranial nerve palsies have been reported. Cranial nerves V-VIII and IX-XII can be involved in patients with RHS, resulting in such symptoms as trigeminal neuralgia, facial palsy, double vision, hearing loss, hoarseness, and tongue deviation [1]. Although the mechanism of cranial nerve involvement remains uncertain, some hypotheses seek to explain it. One hypothesis is anatomical location; on the anterior and posterior regions of the geniculate ganglion the facial nerve joins the vestibulocochlear nerve, and connects with cranial nerves IX and X. Another hypothesis concerns vascular supply; cranial nerves IX-XII are supplied by the ascending pharyngeal arteries and vasculitis caused by viral infections might cause polyneuropathies [2]. IV or oral administration of acyclovir and IV prednisolone are recommended for the treatment of RHS [3]. Analgesic and anti-vertiginous drugs can be used when necessary. It was reported that acyclovir combined with steroid treatment is more effective than acyclovir alone [4]. The prognosis of RHS is worse than that of Bell’s palsy. Moreover, the prognosis of RHS is expected to improve if treatment is started within 3 days of the onset of symptoms. Shim et al. [5] reported that among 328 RHS patients without multineuropathy, 67.7% had complete recovery and 82.9% had complete or partial recovery. In contrary, the partial and complete recovery rates among the 11 RHS patients with multineuropathy were 54.5% and 27.3% respectively. Therefore, they concluded that RHS with multiple cranial involvement was significantly associated with poorer prognosis than RHS without it. Another study on the treatment of RHS that included 80 patients reported that 75% of the patients had total recovery with acyclovir and prednisone treatment that was initiated within 72 hours of symptom onset. In patients in which treatment was started 7 days after symptom onset the complete recovery rate was only 30% [6,7]. Another study reported that RMS patients without diabetes mellitus and hypertension more completely recovered [3]. Cranial nerve X is the most commonly involved cranial nerve in RHS and it can rarely be accompanied by laryngeal eruptions which is an indicator of a rare inflammatory disease called 'herpes zoster laryngitis'. As in the patient 1, herpes zoster laryngitis usually manifests as laryngeal mucosal lesions, erythema and edema on the laryngeal mucosa. It may develop with or without RHS and it is important to exclude possible laryngeal diseases like malignancies, laryngeal tuberculosis and fungal enfections for accurate diagnosis. Steroids and antiviral agents are recommended for the treatment [8]. Although the recovery of facial nerve palsy in patients with RHS accompanied by herpes zoster laryngitis is good, recovery of vagal nerve palsy is poor [9]. In the present study patient 1 had facial palsy for 2 days when she was examined by us and her symptoms completely recovered. On the other hand, patient 2 was referred 5 days after symptom onset and had comorbid diseases—in particular, chronic renal failure caused immunosuppression. Severe aspiration and aspiration pneumonia occurred due to cranial nerve X paralysis. Patient 1 was younger than patient 2 and did not have chronic disease. We think the difference in prognosis between the 2 patients might have been due to comorbidities in patient 2. References
|
|||||||||||||||||||
| Keywords : Ramsay-Hunt sendromu , multinöropati , herpes zoster otikus | |||||||||||||||||||
|