|
|||||
AbstractEpidermal cysts (epidermoid cyst or epidermal inclusion cyst) are a course of neck masses or cervical lymphadenopathies and commonly present head and neck. But only a few reports of inclusion cysts in cervical nodes were found in the literature. We present here a rare case of keratinous cyst in a cervical cymph node diagnosed by ultrasonography. Surgical excision was done and diagnosis confirmed by histopathology. Due to benign inclusions in lymph nodes are very rare and they mistakenly interpreted as tumor metastasis, studies investigating this subject are significant contributions to the literature. For this reason, we proposed practice pathway for cervical lymphadenopathy in children. We also provide a brief review of neck epidermal cysts, histopathological differential diagnosis, and malign transformation.IntroductionThe lymph nodes are an essential part of the body’s immune system and as such are affected in many infectious, inflamatuary, autoimmune, metabolic and malignant processes that appears as neck masses. Cervical lymphadenopathies are a symptom otolaryngologysts in hospitals and surgeries are frequently confronted with among children. As Table 1 shows, there are many possible causes of lymphadenopathies [1,2]. For this reason, history and through clinical examination with a laboratory and radiological assessment are crucial steps towards securing a diagnosis1. Enlarged lymph nodes must be differentiated from all these possible causes of neck masses, also epidermoid cysts (epidermal cysts or epidermal inclusion cysts or dermoid cysts) [3]. Epidermal cysts are a course of neck masses or cervical lymphadenopathies, and these cysts are the simplest germ cell layer lesion, consisting of only a single layer of ectoderm. Historically the most common type is known as an epidermoid cyst or epidermal inclusion cyst. This contains approximately 90% of keratinous cysts which characterized by cornified epithelium, a very well demarcated granular layer, and multiple lamellae of keratin without calcification [3]. Furthermore focal calcification is common [4]. In the presence of benign inclusions in lymph nodes, the most worrisome feature of these benign inclusions in lymph node is that they may be commentated as tumor metastasis mistakenly [5,6]. Therefore, the awareness of such an entity is all the more important in preventing overdiagnosis of malignancy. Total surgical excision is required with care taken to completely remove the enlarging mass and the cyst wall, and to minimize spillage of cyst ingredients to prevent it’s recurrenc [7]. Also complete excision of lymph nodes at an early stage will both confirm the diagnosis and eradicate the disease. To our knowledge, this is a very rare case of a cervical lymph node in literature. This case report indicates that clinicans should be aware that cervical keratinous cysts, although it is uncommon, can be a cause of lymphadenopathy or neck abscess. We conclude that keratinous cysts in cervical area may be a presentation and should be kept in mind for differential diagnosis. A review of the literature and a proposed practice pathway for cervical lymphadenopathy in children is reported. We also provide a brief review of neck epidermal cysts, histopathological differential diagnosis, and malign transformation. Case ReportA 10-year-old girl living in poor social conditions presented for evaluation of a left neck mass with diameter of about 4x2 cm and with intense inflammatory reaction of the surrounding neck tissues. There was no history of trauma or any previous surgery or tuberculosis. The mass had been present from about 3 weeks with a gradually increasing volume but without fever and little pain. Twice, she received antibiotic treatment with amoxicilin and clavulanic acid (1 g BID for 7 days) with partial resolution of pain and reduction in mass volume. ENT examination observed a neck mass at left level IIA; it was palpable, round, and poorly mobile on both deep and superficial planes with the consistency of an inflamed lymph node. No movement with swallowing or protrusion of the tongue could be demonstrated. Several adjacent smaller lymph nodes were found. The skin over the mass showed minimal redness and felt warm to the touch. Other side of servical region was normal. On general physical examination, no other swelling was noted elsewhere in the body. Chest X-ray was negative for pulmonary tuberculosis but Mantoux test (Tuberculin skin test ) revealed an induration of 11 mm. Ultrasound scan documented an “oval mass of about 45×25 mm with hypoechoic echo structure with sporadic hyperechoic spots and intralesional flow signals. Reactive lateral cervical lymphadenopathy”. Complete Blood Count (CBC) analysis demonstrated high white cell count (14.90 × 10[9]/L; normal range: 5.0-8.0) in neutrophil dominance (8.42 × 10[9]/L; normal range: 2.0-6.0). Other blood test on admission showed no remarkable abnormalities in, hemoglobin (14.0 g/dL; normal range: 13.5-17.5), platelet (196 × 10[9]/L; normal range: 120-280), and lactate dehydrogenase (150 U/L; normal range: 100-210). High CRP (7,8 mg/dl; normal range: less than 0.3) was noted. Serum HBs antigen, HIV, HCV, EBV, Toxoplasmosis IgM, IgG antibody results were negative. The mass also presented centrally cystic- necrotic component. On the basis of the clinical examination, a provisional clinical diagnosis of tuberculous lymphadenopathy was made. To confirm our diagnosis, surgical excision of the cyst was then planned under general anesthesia. The specimen was sent for histopathological examination (Figure 1).
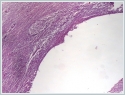
Pathologic analysis revealed cyst lined by stratified squamous epithelium with preserved granular layer with retention of keratinous debris suggestive of epidermoid cyst with an active inflammation (Figure 2). There were no histological findings of malignancy and no microbiological signs of atypical mycobacterium. There were no signs of recurrence during the 6-month follow-up period.
DiscussionCervical lymph node swelling of uncertain origin in childhood can pose a special difficulty to the attending pediatric and ENT physicians [8]. They must follow a clearly structured algorithm in their therapeutic strategies and diagnostic steps (Figure 3: Algorithm of lymph node diagnosis) [1]. Primary diagnostic instruments such as history and clinical examination are very important for the physicians because of there are various possible differential diagnoses [9,10].
The history must include any reference to a focus, including in the past, such as a throat ache, earache or toothache, insect bites or injuries. Details of foreign travel, possible contact with animals (in particular cats, rabbits, rodents, tick bites), equally of all vaccinations and family history must also contain in the history [10,11]. Clinical examination of the young patients initially includes inspection, palpation, ENT examination and more extensive examinations as indicated, comprising palpation of other lymph node regions (axillary, inguinal etc.) or of the spleen and liver [9]. If the history and clinical examination prove inconclusive, or if confirmation of a suspected diagnosis is required, further diagnostic means are available, containing serological tests, sonography as the basic imaging technique, and for certain special indications also MRI and CT [9,10]. In the presence of suspicious lymph node, complete resection should take preference over fine-needle aspiration cytology (FNAC) to obtain histological confirmation [12]. Laboratory diagnosis is generally used in lymphadenopathy of indefinite origin. Parameters such as the erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) and lactatedehydrogenase (LDH) are observed higher in many infectious but also immunologic and neoplastic diseases and therefore tend to be nonspecific [9]. To confirm a suspected malignancy, a blood count including microscopic differential hemogram can further help [13]. Once the diagnosis has been established, the laboratory tests are used to define which organs are involved in systemic diseases. depends to a critical degree on the quality of the material submitted for testing effects the success of microbiological diagnosis. Serology is primarily used to establish diagnosis for virus-associated diseases. If antibiotic treatment has already begun, blood cultures are considerably less reliable, since antibiotic substances continue to work in the culture bottles and may hinder pathogen growth [9]. Tuberculin skin test can used to diagnose tuberculosis [9]. Imaging techniques are used in cervical lymph node swelling in children to confirm or eliminate a specific diagnosis (e.g. abscess) or to assess the location and number of affected structures and can significantly contribute to diagnosis where clinical assessment and history are inconclusive [9]. Sonography is a very valuable way to assess lymph node swelling in pediatric age group, and provides answers to a range of questions in differential diagnosis and standard choice of imaging procedure [14]. In inflamed processes, sonography is the instrument of choice for determining localization, size, number and characteristic properties of the affected structures [15,16,17]. A CT scan provides morphological evidence to confirm the lymphadenopathy, primarily by size, shape and, infiltration of the surrounding structures in advanced stages. Magnetic resonance imaging (MRI) can above all help to identify neck masses not originating in the lymph nodes and is a further procedure available as part of more extensive diagnosis [9]. If malignancy is suspected or a condition persists histological examination is warranted without too much delay in which case the complete resection of the affected lymph node is gold standard [18]. A fine-needle biopsy is an option if (i) several lymph nodes are suspicious, (ii) surgical dissection is associated with a high risk that can be eliminated by FNAC, (iii) sufficient expertise is available, and (iiii) the patient is in compliance (age of the patient!) [9,19]. Detailed morphological evaluation of lymph nodes is crucial in reaching at an accurate diagnosis as these inclusions may be misdiagnosed as tumor metastasis. The criteria favoring benign inclusions include bland nuclear cytology, absence of anaplasia, brisk mitosis, and necrosis [20]. Epidermoid cysts are common subcutaneous cysts that can occur anyplace in the body and 7% of them occur in the head and neck. It is defined as “A simple cyst lined with stratified squamous epithelium and lumen is filled with keratin or cystic fluid and no other specialized structural property.” [21]. Various theories have been proposed to explain the origin of epidermoid inclusion cysts (congenital, acquired) until now, but previous surgery or trauma should always be excluded first [22]. Congenital cysts develop due to abnormal sequestration of surface ectoderm at embryonic fusion site or due to failure of separation of ectoderm from underlying neural tube. Acquired cyst arises from the inclusion of epidermal structures into dermis and deeper tissue, like trauma [23,24]. Our patient did not report any congenital neck mass or previous surgery. Epidermoid cysts usually become apparent in patients between 15 and 35 years but they can occur at any age from birth to 72 years. Males are affected more commonly. Multiple epidermal cysts can occur but these are usually solitary, and may present as small or large masses [24-26]. Servical Epidermoid cysts can reach large size rarely. In the literature, problems such as compression, swallowing difficulty and/ or breathing or recurrent infection are determined [27,28]. The size of the cyst is so important because of giant cysts (>5 cm) have more risks of malignant transformation as compared to conventional cysts [29]. The present case is case of a 10 year old girl with small solitary keratinous cyst in cervical lymph node. Servical epidermoid cysts grow slowly and do not cause symptoms usually. Most cases are placed in the midline of the neck and in the submental area, present as superficial masses that move with the skin without pain. They will grow slowly but will become infected occasionally. In the present case, the mass was poorly mobile and inflammatory [30]. Radiographic examinations such as ultrasound scans may be misleading when a cyst is infected [29] because in the presence of infection, sonographic features can be similar to tuberculous lymphadenopathy. First, we suspected tuberculosis due to our patient’s low socio-economic situation. With a positive Mantoux test this hypothesis was supported. But a positive test is not diagnostic for tuberculosis, as atypical mycobacterial infection may cause false positive results. However A negative Mantoux test is reassuring. As in our patient, ultrasound scan can lead to an incorrect diagnostic hypothesis and can be misleading. Thus, epidermoid cysts should be kept in mind in the differential diagnosis of a cystic neck mass although they are not uncommon in the pediatric population [31]. Possibility of secondary malignancy occurance within the cyst makes these diagnostic importance. Squamous cell carcinoma is the most common malignancy associated with the epidermoid cyst and Basal cell carcinoma is the second most common malignancy occurring from this cyst. The most common risk for the development of squamous cell carcinoma is exposure of the skin to ultraviolet radiation. Also HPV infection has been stated as one of the risks. Squamous cell carcinoma is more likely to develop in a chronically diseased or injured skin [32]. Lymph nodes with benign inclusions were first described by Ries in 1897 [6], Brooks et al.[7] classified them into three different types as epithelial, nevomelanocytic and decidual. Epithelial cells in these inclusions may germinate from squamous epithelial cells, salivary gland tissue, breast tissue or thyroid tissue, etc. The type of heterotopic inclusions effects which lymph nodes involved most commonly. Thyroid tissue and salivary gland tissue are commonly found in cervical nodes [5,6]. On extensive search of the literature, we encountered only a few reports of inclusion cysts in cervical nodes [33,34]. We considered it worthwhile to report this rare occurrence in a servical lymph node to create awareness about the existence of such an unusual benign entity in a lymph node among otolaryngologysts. Awareness of this rare entity can prevent misdiagnosis of a tuberculous lymphadenopathy or malignancy and thereby prevent unneeded treatment. Financial support and sponsorship: The authors received no financial support for the research and/or authorship of this article. Conflicts of interest: The authors declared no conflicts of interest with respect to the authorship and/or publication of this article. Patient consent: Written informed consent was obtained from the patient’s mother for publication of this case report and accompanying images. Authors’ contributions: ASA was the principal author and major contributor in writing the manuscript. DS and DN performed the histological examination of the keratinous cyst. All authors reviewed and approved the final manuscript. AcknowledgementWe thank Hilal Kayahan for her help in English revising on this manuscript. References
|
|||||
| Keywords : keratinöz kist , lenfadenopati , epidermal inklüzyon kisti , boyun kisti , çocuk | |||||
|