|
|||||
AbstractPrimary lymphoma is an uncommon malignancy of the thyroid, comprising between 1 and 5 per cent of thyroid cancers It typically presents as a rapidly enlarging goiter with associated compressive symptoms. Thyroid ultrasound and fine needle aspiration cytology and immunohistochemistry, remain the main modalities used to confirm the presence of lymphoma. The majority of thyroid lymphomas are diffuse large cell of B-cell origin. The prognosis is generally excellent but can be varied because of the heterogeneous nature of thyroid lymphomas. We report two cases of primary thyroid lymphoma and highlight the clinical issues and challenges posed by this rare disease.IntroductionPrimary thyroid lymphoma [PTL] is 1 to 5% of all thyroid malignancies, and 1 to 2% of extranodal lymphomas. The incidence of PTL peaks in the fifth and seventh decades of life. This tumor type is three-fold more frequent in females compared to males [1-2]. The most common symptom at presentation is a rapidly growing neck mass with accompanying dysphagia. Thyroid function tests are often normal [euthyroid] in most patients. The tumor mass is often adherent to the surrounding tissues and half of the patients have unilateral or bilateral lymph node involvement. Distant metastases, however, are rarely observed [3]. The incidence of Hashimoto’s thyroiditis ranges from 25 to 100% in patients with PTL [4,5]. Thyroid lymphoma is generally seen as non-Hodgkin lymphoma type. Fine needle aspiration biopsy can hardly differentiate it from an anaplastic carcinoma [3]. As a result, this poses a challenge in the diagnosis and treatment of the disease. Herein, we report two cases with PTL in whom the diagnosis was challenging. Case ReportCase Report 1 A 62-year-old male patient was admitted to the outpatient clinic with the complaint of a lump on his neck. Otorhinolaryngological examination revealed a neck mass in left tyhroid gland lobe. Complete blood count and biochemistry revealed normal findings. Thyroid function tests showed a thyroid stimulating hormone (TSH) level of 22.46 (0.27-0.42) mIU/mL, free T3 of 2.33 (2-4.4) mIU/mL, and free T4 of 0.717 (0.9-1.7) mIU/mL. Neck ultrasonography showed an approximately 5-cm nodular lesion occupying the left thyroid gland lobe. Neck computed tomography (CT) revealed a 50-53-mm soft tissue mass communicating with the left thyroid gland lobe and displacing neurovascular structures on the left (Figure 1).
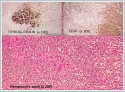
Pathological examination of the fine needle aspiration biopsy specimen showed the suspected metastatic lymph node from the thyroid tumor or a simple thyroiditis exhibiting lymphoid reaction or thyroid lymphoma. A written informed consent was obtained from the patient, and then he underwent total thyroidectomy with frozen-section examination. Frozen-section of the left thyroid lobectomy material showed positive results for malignancy, and the patient underwent total thyroidectomy. No complication was observed periopratively and in postoperative term. CD20 was investigated by immunohistochemical methods. Malignant cells show staining with CD20 and postoperative histopathological examination of the specimen showed diffuse large B-cell lymphoma. The patient was, then, referred to oncology outpatient clinic for staging and administration of additional therapies. And informed consent for publication was obtained from the patient. Case Report 2 A 70-year-old female patient was admitted to the outpatient clinic with the complaint of a lump on the right side of her neck. Otorhinolaryngological examination revealed a neck mass in the right submandibular area and right thyroid gland lobe. Complete blood count, biochemistry, and thyroid function tests revealed normal findings. Neck ultrasound showed a prominent hypoechoic nodule in the right thyroid gland lobe measuring 28x24 mm in size. There were also multiple hypoechoic lesions with well-defined margins, the largest measuring 15x12-mm inferior to the thyroid gland and 35x30-mm at 2A level in the right jugular cervical area. Neck magnetic resonance imaging (MRI) showed a solid nodular lesion in the right thyroid gland lobe measuring 30x25 mm in size. There were solid lesions on cervical lymph nodes, the largest measuring 45x30 mm in size located on the right posterior submandibular level with peripheral contrast uptake following intravenous contrast injection, and some exhibited homogeneous contrast uptake. Histopathological examination of the thyroid fine needle aspiration biopsy specimen failed to show thyrocytes; however, malignancy and lymphocytic thyroiditis were unable to be ruled out due to the cellular pattern of the lymph node with irregularly-shaped, large, swollen nuclei related to the diffuse degeneration and inconspicuous nucleoli. Histopathological examination of the fine needle aspiration biopsy specimen of the cervical lymph node showed vivid cellular elements in a small area of the lymph node smear, suggesting reactive changes. A written informed consent was obtained from the patient, and then she underwent total thyroidectomy with frozen-section examination and right functional neck dissection including sixth level was performed. Frozen-section examination of the lymph node located in the submandibular area was performed during neck dissection, suggesting lymphoma. Then, the right thyroid gland lobe was removed and sent for frozen-section examination, suggesting an anaplastic carcinoma. The patient, then, underwent total thyroidectomy with right functional neck dissection. No complication was observed perioepratively and in postoperative term. CD20 was investigated by immunohistochemical methods. Malignant cells show staining with CD20 and postoperative histopathological examination of the specimen showed diffuse large B-cell lymphoma(Figure 2).
DiscussionPrimary thyroid lymphoma is a rare tumor with the peak incidence in the fifth and seventh decades of life. In the clinical presentation, these lesions manifest as rapidly growing diffuse thyroid masses in elderly women with history of chronic lymphocytic thyroiditis [3, 6]. The patients may also suffer from hoarseness, stridor, and dysphagia. Less than 20% of the patients may also have fever, night sweats, and weight loss which is known as B symptoms [7]. In our both cases, the chief complaint at presentation was a neck lump. There were no additional symptoms. In addition, the ages of the patients were consistent with the literatüre [1-2]. The majority of PTLs are seen as B-cell non-Hodgkin type that characteristically in patients with autoimmune thyroiditis, while primary Hodgkin lymphoma of the thyroid gland is extremely rare. Primary non-Hodgkin lymphomas of the thyroid gland is diffuse large B-cell lymphoma [DLBCL], and it is the most common type with the incidence of 70 to 80%, followed by marginal zone B-cell lymphoma [MALT] with an incidence of 15 to 30% [8]. Pathological examination revealed DLBCL in our cases. Due to the common occurrence of Hashimoto’s thyroiditis, thyroid peroxidase antibodies [Anti-TPO] are largely positive in these patients [8]. Although most patients are euthyroid, apparent or subclinical hypothyroidism can be commonly seen [9]. One of our cases was euthyroid, while the other had hypothyroidism. Radiological imaging of the thyroid gland does not yield specific findings in cases with PTL. Several studies reported that MRI could differentiate Hashimoto’s thyroiditis from thyroid lymphoma [10]; however, there are also publications in the literature reporting no utility of the MRI in the differential diagnosis [11]. Some authors also found that thyroid lymphomas may appear radiologically similar to thyroid adenoma or carcinoma [12]. Although fine needle aspiration biopsy is one of the mainstay procedures in thyroid masses, it is effective in 60% patients with thyroid lymphoma [13]. Thyroid lymphomas typically occur in patients with small-cell carcinoma of the thyroid gland and Hashimoto’s thyroiditis; therefore, they can be frequently misdiagnosed [3]. Compared to the pathological examination of the surgical specimens, frozen-section of hematolymphoid tissues yields limited data and, therefore, frozen-section is not recommended as a diagnostic procedure. Artificial changes in the cellular morphology related to the freezing of the tissues even complicate the basic differentiation of benign from the malignant tissues [13]. In our cases, surgery accompanied by frozen-section examination was planned due to the limited benefit of fine needle aspiration biopsy. The first case underwent total thyroidectomy, as frozen-section examination showed malignancy. In the second case who underwent total thyroidectomy with functional neck dissection to the affected side, while frozen-section examination of the lymph node suggested lymphoma, the examination of thyroidectomy specimen showed that raised the suspicion of anaplastic carcinoma. The first case was diagnosed as primary tumor due to the lack of peripheral lymph nodes. However, primary or metastatic tumor differentiation was unable to be performed in the second case due to the presence of multiple lymph nodes. Furthermore, surgery is the primary treatment of choice in patients with differentiated thyroid malignancy. This principle, however, does not apply to patients with anaplastic carcinoma and PTL. Radiotherapy and chemotherapy are first-line treatment options in these patients. The role of surgery is limited by only resection for diagnostic purposes and maintaining airway patency [3, 14-15]. Due to relatively rare occurrence of PTLs compared to other thyroid malignancies, thyroid lymphoma is not considered initially in the differential diagnosis of thyroid masses. However, PTL should be considered in the differential diagnosis, particularly in the presence of symptoms such as a rapidly growing thyroid mass, hypothyroidism, chronic lymphocytic thyroiditis, and obstructive symptoms. Fine needle aspiration biopsy is the initial method which can be applied in the differential diagnosis, although its yield may be limited. Histopathological examination of the surgical specimen provides the definitive diagnois, and radiotherapy and chemotherapy is the optimal therapeutic option in this patient population. References
|
|||||
| Keywords : Tiroid lenfoma , primer , patoloji , malign tümör | |||||
|