|
|||||||||
AbstractThe most common complications of direct laryngoscopy, which is an indispensable part of otolaryngology practice, are minor mucosal lesions. Rarely, hypoglossal nerve, vocal fold, and lingual nerve palsies may occur. This case presentation is about unilateral hypoglossal nerve palsy following direct laryngoscopy. A 60-year-old-man was admitted with a complaint of hoarseness for 3 months. Direct laryngoscopy and biopsy of the right vocal fold were performed with the preliminary diagnosis of glottic cancer. The day after surgery, he complained of dysphagia. The tongue deviated to the left side of the tongue while protrusion with hypotonia of the left anterior two-thirds. Computerized tomography was performed to exclude hematoma, regarding anticoagulant use before surgery. The palsy completely recovered after 2 months of surgery without any treatment. Shifting of laryngoscope from the midline to the left side for better visualization of the right vocal cord may be the reason for this palsy. Care should be taken to keep the laryngoscope in the midline as much as possible during surgery.IntroductionDirect laryngoscopy (DL) is one of the most common practices of otolaryngology. Minor mucosal lesions are the most common complications of DL [1]. Hypoglossal nerve palsy (NHP), which may occur after intubation, laryngeal mask airway, tonsillectomy, and carotid endarterectomy, is a rare complication of DL [2-5]. We present a case with HNP after DL in view of the literature. Case ReportA 60-year-old man was admitted to our clinic with a complaint of hoarseness for 3 months. In the endoscopic examination, there was erythroplakia on the right vocal cord with anterior commissure involvement, but the movement of the cords was normal. According to his medical history, the patient smoked 30 year/packs and he was on acetylsalicylic acid, clopidogrel, and metoprolol for coronary heart disease. Before surgery, cardiology consultation had been taken. DL with Kleinsasser anterior commissure laryngoscope (Karl Storz, Germany) and biopsy was performed from the right cord under general anesthesia (Figure 1).
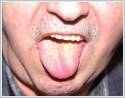
The day after surgery, he complained of mild dysphagia. There was a deviation to the left side of the tongue while protrusion with hypotonia of the left anterior two-thirds in his physical examination (Figure 2).
The result of pathology from right vocal cord was “squamous cell carcinoma”. After consultation about treatment options with patient surgical treatment was planed. Because of the hypoglossal nerve palsy complication of the prior intervention, open right frontolateral partial laryngectomy was performed without any complication. After 2 months follow up, the HNP recovered totally without any treatment (Figure 4).
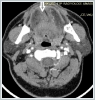
DiscussionThe hypoglossal nerve emerges from the medulla oblongata and enters the hypoglossal canal, moving downwards between the great veins of the neck to the mandible angle. It then moves below the digastric muscle, penetrates the oral cavity and innervates all the intrinsic and extrinsic tongue muscles, except the palatoglossal muscle. The course of the nerve and proximity to hyoid bone makes the nerve vulnerable. The incidence of HNP as a complication of DL is %1.1 [1]. Some situations such as operation time, the pressure to cricoid for better visualization, hyperextension of the neck can be other factors of HNP [6, 7]. Lingual nerve palsy may also occur with or without HNP after oropharyngeal operations or intubation [6]. Besides, recurrent laryngeal nerve paralysis and HNP may occur together as an intubation complication described before [8]. The treatment of HNP is unclear in the literature. A short course of high-dose steroids such as prednisone may be advocated if airway edema is suspected [9]. As to nerve function recovery, there are reports of improvement after 8 weeks for hypoglossal nerve injuries as in our case [7]. We thought that hematoma of the tongue base may be a cause for the paralysis due to the anticoagulant drugs used for the current cardiac disease. But we have ruled this out by physical examination and radiological examination. Shifting of laryngoscope from the midline to the left side for the best visualization of the right vocal cord may be the cause of palsy in our case. The nerve can be compressed between the laryngoscope and the hyoid bone or calcified stylohyoid ligament [10]. Unlike other cases published before, the HNP may change the surgical approach due to the probability of permanent palsy and risk of dysphagia after laser surgery as in our case. In conclusion, during DL, care should be taken to keep the laryngoscope in the midline as much as possible. References
Presented atThe case was presented in the 38th National Otorhinolaryngology-Head & Neck Surgery Congress as an e-poster presentation, 26-30 October 2016- Ankara, Turkey. |
|||||||||
| Keywords : Larenks neoplazmları , larengoskopi , hipoglossal sinir yaralanmaları | |||||||||
|