|
|||||||||||||
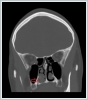
AbstractInverted papilloma (IP) is one of the benign sinonasal tumors and usually originates from lateral nasal wall mucosa. Despite being a benign tumor, IPs might invade neighboring structures such as paranasal sinuses, orbita, even skull base. IPs are known for high recurrence rates after incomplete resection. Due to this important feature of tumor, total resection of the tumor is a must for optimal treatment. Technological advancements within recent years made transnasal endoscopic techniques new gold standard for patients with limited disease.Fontanelle area of lateral nasal wall is the most common location for inverted papilloma. There are hardly any report for any cases having isolated inverted papilloma of the inferior turbinate without involvement of middle meatus in current literature. This paper reports a rare presentation of isolated inverted papilloma at inferior turbinate and aims to increase our knowledge about this common sinonasal tumor. IntroductionInverted papilloma (IP) is one of the benign sinonasal tumors and usually originates from lateral nasal wall mucosa[1]. Despite being a benign tumor, IPs might invade neighboring structures such as paranasal sinuses, orbita, even skull base. IPs are known for high recurrence rates after incomplete resection. Furthermore, recurrent tumors are more prone to invade adjacent anatomical structures. Due to this important feature of tumor, total resection of the tumor is a must for optimal treatment. For total resection, surgeons had preferred more aggresive approaches like medial maxillectomy through lateral rhinotomy or midfacial degloving, but technological advancements in otolaryngology in recent years allowed us to use more conservative techniques, such as transnasal endoscopic tumor resection, in most patients[2] . Fontanelle area of lateral nasal wall is the most common location for inverted papilloma[1]. Boundaries of fontanelle area are lacrimal bone anteriorly, perpendicular plate of palatine bone posteriorly, orbital floor, bulla ethmoidalis and ground lamella of the middle turbinate superiorly, superior border of the inferior turbinate inferiorly[3]. The maxillary sinus is the second most common location for IP and frontal and sphenoidal sinuses are rare involvement areas[1]. There are hardly any report for any cases having isolated inverted papilloma of the inferior turbinate in current literature. In a recent study, authors reported an unexpected IP diagnosis of inferior turbinate in a patient underwent functional endoscopic sinus surgery for nasal polyposis[4]. As far as we know, there are no case with isolated IP located in inferior turbinate, without involvement of middle meatus; thus this paper reports the first patient. Case ReportA 34-year-old female patient, who was misidentified for hemoptysis, was consulted from Pulmonogy clinic. The patient had a history of intermittent posterior epistaxis and post-nasal dripping for several months. There was no nasal stuffness, discharge or anterior epistaxis complaint. Anterior rhinoscopy showed no pathologies, yet nasal endoscopy revealed a firm, greyish and polypoid mass attached to posterior part of right inferior nasal turbinate (Figure 1).
Operation was performed under general anesthesia, with 0[0] 4 mm rigid nasal endoscope. The posterior portion of right inferior turbinate which was the mass was attached, was resected with clear surgical borders. Bleeding control was completed with bipolar cauterization. Removed mass was a piece of 2x0.5 cm in size, with a polypoid shape, elastic consistency and grayish-brown color (Figure 3). A benign tumor of nasal cavity thought as initial diagnosis and patient was scheduled for endoscopic total resection of the tumor.
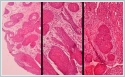
Microscopical histopathologic examination revealed, tissue had structurally prominent downward endophytic growth of round to elongated interconnected epithelial nests with smooth outer contour in hemotoxylin eosin (HE) stained sections (Figure 4). Epithelium was hyperplastic squamous and transitional type (Figure 4).There were neutrophils infiltrating the epithelium and stroma, and chronic inflammation in the stroma (Figure 4). Seromucinous glands in the lamina propria was absent.
Patient is still being followed-up with transnasal endocopical examinations. After 1 year, there’s no recurrence at operation site as seen on Figure 5 and patient is symptom-free.
DiscussionInverted papilloma is the second most common sinonasal benign tumor and it originates from Schnederian ectodermal mucosa of the nasal cavity[1]. Even though being a benign tumor, IPs can be locally aggresive and invade surrounding structures like paranasal sinuses, orbita and intracranial space through bone erosion. It’s diagnosed mostly in fifth - sixth decades of life and men are more commonly affected than women[1]. Etiology is still unclear, but smoking and human papillomavirus (HPV) are considered as possible causes[5]. IPs are associated with squamous cell carcinoma and with a 3.4 – 9.7% prevalance and synchronous occurence[1]. Fontanelle area of lateral nasal wall is the most common location for inverted papilloma[1]. The maxillary sinus is the second most common location for IP and frontal and sphenoidal sinuses are rare involvement areas[1]. Although “lateral nasal wall” involves inferior turbinate in classification systems for IP, isolated IP on inferior turbinate without middle meatus involvement is a rare presentation. Reviewing of literature, only report for IP on inferior turbinate, Carta et al. reported an unexpected IP located on inferior turbinate, which was misidentified for a nasal polyp in a patient with nasal polyposis[4]. Still, our case didn’t have nasal polyposis, only an isolated inverted papilloma. The most common symptoms of IP are nasal obstruction, epistaxis, rhinorrhea and anosmia. In extensive disease with orbital or skull base involvement; epiphora, diplopia, proptosis and headache could also be main symptom. Diagnosis may be tricky with some cases like our patient who had posterior epistaxis that misidentified as hemoptysis. Nasal endoscopy is a must in diagnosis. IPs are generally seen as polypoid, pale mass with a papillary appearance that bulges out of middle meatus. Endoscopic biopsy should be performed for histopathologic diagnosis. Hyperplastic epithelial cells growing into underlying stroma with a intact basal membrane and cellular atypia at variable rates are generally seen in histopathologic specimen[6]. In our patient, considering isolated and free nature of mass, we performed total excision for tumor for both diagnosis and treatment. In evaluating extent and three-dimesional configuration of the lesion, computed tomography (CT) and magnetic resonance imaging (MRI) are valuable options in imaging. Relationship with vital surrounding structures like internal carotid artery, optic nerve, skull base and orbit must also be assessed in imaging studies. CT is more successful for showing bone erosion, yet MRI is the better choice for showing extension of tumor[7]. T2-weighted MRI is successful for distinguishing IP from surrounding inflammatory response, whereas T1-weighted MRI is the better choice for determining the orbital or nasopharyngeal invasion[7]. Considering that extension of disease is the primary factor for planning surgery, MRI is crucial in extensive disease with multiple space involvement such as paranasal sinuses, orbit or intracranial space. Recent studies had shown osteitic changes and focal hyperostosis in CT may be considered positive predictors of tumor origin[8, 9]. In imaging of our case, CT showed a mass located on right inferior turbinate without any evidence for middle meatus involvement or sinusitis. Considering isolated and free mass on inferior turbinate, as clearly seen on nasal endoscopy, we didn’t need MRI for assessing extent of tumor thus MRI wasn’t performed. It has been shown in studies that IPs may transform in to malignant disease with %5-15 ratio[10]. Risk factors for malignant transformation are still unclear. For this reason, clinicians are usually unable to foresee the malignant potential of IPs, even with biopsies. Taken all together, uncertain nature of malignancy, tendency to recur after incomplete resection and infiltrative nature of IPs requires total resection of the tumor at first approach. Primary treatment of IP is surgery. Before the nasal endoscopes had become widespread, gold standard techniques were external approaches, usually paralateronasal techniques combined with medial maxillectomy[11]. Technological advancements within recent years made transnasal endoscopic techniques new gold standard for patients with limited disease. Endoscopic surgery offers many advantages such as reduced operation time, avoiding visible scars and shorter post-operative hospitalization. However, external or combined external/endoscopic approaches remain indicated for extensive disease. Lesions at lateral wall of nasal cavity, ethmoid or sphenoid spaces could easily removed totally with endonasal endoscopic approach. Endoscopic technique is also sufficient for removal of IPs at medial, superior or posterior walls of maxillary sinus. However anterior, inferior or lateral wall of maxillary sinus involvement usually need combined endoscopic and Caldwell-Luc approach for complete resection of tumor. Frontal sinus is also a hard location to remove IPs only with endoscopic techniques. Frontal osteoplastic flap should be added to endoscopic technique for removal of IPs, especially with lateral wall of frontal sinus involvement. Extrasinusoidal extension of IP or associated malignancy is usually preferred to treated with external approach, such as paralateronasal techniques. Our patient had a isolated IP located on posterior part of inferior turbinate and showing no evidence of malignancy, so we preferred transnasal endoscopic approach for total removal of tumor. Patients with IP must be followed-up after surgery for at last 5 years minimum[11]. Some authors recommend a lifetime follow-up, considering late recurrences and metachronous carcinomas[11]. Follow-up examinations comprises mostly nasal endoscopy, radiological studies and punch biopsies if required. IP in our case localised at a highly visualised anatomical site, so endoscopic examination was sufficient for our follow-up examinations. Our patient is disease-free without symptoms for 1 year. In conclusion, inverted papilloma is a benign sinonasal tumor and definite etiology of IP is still unknown. IPs are tend to recur after incomplete excision and have risk of carcinomatous progression, thus total surgical resection is a must for treatment. Endonasal techniques are gold standard for treating limited disease and prolonged follow-up duration after surgery is recommended by latest studies. This paper reports a rare presentation of isolated inverted papilloma and aims to increase our knowledge about this common sinonasal tumor. References
|
|||||||||||||
| Keywords : inverted papillom , alt konka , endoskopik , izole | |||||||||||||
|