|
|||||
AbstractChronic lymphocytic leukemia (CLL) is a chronic lymphoproliferative disorder described as a clonal proliferation and expansion of B cells in the blood, lymphatic organs, and lymph nodes.Leukemic infiltration of paranasal sinus involvement is extremely rare for CLL patients. Also, they have a tendency to paranasal sinus infections. Each CLL patient with paranasal sinus involvement must be individualized for treatment. CLL patients with rhinitis symptoms need to be performed a paranasal sinus biopsy via the endoscopic sinus surgery by otorhinolaryngologists to be diagnosed with the relapse or not. In this case report, the 7th case of CLL involving the paranasal sinuses mimicking chronic rhinosinusitis was presented with the light of the current literature. IntroductionChronic lymphocytic leukemia (CLL) is a chronic lymphoproliferative disorder described as a clonal proliferation and expansion of B cells in the blood, lymphatic organs and lymph nodes. CLL is the most common leukemia type seen in adults in Western countries. Males are affected more than females with a 1.7/1 ratio and the median age is 72 [1]. CLL is usually diagnosed with incidental lymphocytosis found in the routine complete blood count (CBC) sampling for any reason. Swelling, non-tender lymph nodes in the physical examination and computed tomography (CT) scans for the neck and thorax region may aid in diagnosis. Additionally, the accumulation of mature B-cells should be confirmed by flow cytometry for the definitive diagnosis [1] . Immunosuppression with hypogammaglobulinemia is commonly associated with CLL. [2,3] Thus, patients with CLL have a tendency to paranasal sinus infections [2]. However, leukemic infiltration of the paranasal sinuses for patients with CLL is extremely rare. In this case report, we presented the 7th case of CLL involving the paranasal sinuses mimicking chronic rhinosinusitis with the light of the current literature (Table 1). We discussed the importance of paranasal sinus biopsy for patients with CLL having rhinitis symptoms. Case ReportA sixty-one years old man with 12 years’ history of the CLL presented with green-colored purulent nasal discharge, nasal congestion and facial pain. His symptoms had been existing for 10 months and many medical treatment options including oral amoxicillin-clavulanate (Augmentin; Glaxosmithkline pharmaceuticals, Istanbul, Turkey) cephalosporins and quinolones had been already given by different physicians in other institutions. Nasal endoscopy demonstrated seropurulent secretions in the middle meatus bilaterally, in addition to the inflamed nasal mucosa. There was no necrosis or eschar tissue as a sign of fungal sinusitis on examination. A computed tomography (Aquillion 64, Toshiba Medical Systems Tokyo, Japan) scan of the paranasal sinuses was performed showing thickened soft tissue in the maxillary and ethmoid sinuses and the obstruction in the ostium of maxillary sinuses bilaterally (Figure 1).
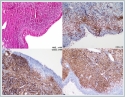
In his past medical history, he was diagnosed as CLL for the first time in 2007. He had received 6 cycles of chemotherapy regimen that he doesn’t know the names and details, in another institution. He was diagnosed as the recurrence of CLL in 2013 in Hematology clinic of our University Hospital. Chemotherapy regimen including rituximab (Mabthera; Roche Diagnostics, Istanbul, Turkey) and cyclophosphamide (Endoxan; EIP Eczacibasi Medical, Istanbul, Turkey) was given in 6 cycles. In 2019, Ibrutinib (Imbruvica; Johnson&Johnson Medical, Istanbul, Turkey) was added to the treatment protocol , given 420 mg by oral route once daily. He had been using Ibrutinib for 8 months. His white blood cell count was 16.91 x 10[3] µl, hemoglobin level was 11,1 g/dL, and platelet count was 147 x 10[3] µl. The patient underwent endoscopic sinus surgery in our tertiary center otorhinolaryngology department since he did not have any relief of symptoms despite numerous medical treatment modalities. Unsinectomy, maxillary antrostomy, anterior and posterior ethmoidectomies were performed bilaterally. During the surgery, polypoid inflamed mucosa was seen, and tissue culture was also taken. Pathologic examination of the surgical specimen showed atypical lymphoid cell infiltration of the mucosa with focal staining of CD3 and diffuse staining of CD20 and CD23 compatible with chronic lymphocytic leukemia (Figure 2).
Methicillin resistant coagulase negative staphylococcus (MRCNS) growth was seen in the tissue culture. The patient received oral levofloxacin (Lefox; VEM Pharmaceuticals, Istanbul, Turkey) 750 mg daily for 2 weeks for MRCNS infection and nasal steroid containing fluticasone furoate for mucosal edema after surgery. Three weeks after surgery his symptoms diminished significantly. As a result of the diagnosis of relapsed CLL in the paranasal sinuses, a whole-body positron emission tomography-computed tomography (PET-CT) scan was performed after the Hematology department consultation. Since he had no other organ involvement on PET scan and he had stable blood counts on the follow-up visits, he didn’t receive any chemotherapy regimen. He continued receiving Ibrutinib (Imbruvica; Johnson&Johnson Medical, Istanbul, Turkey) 420 mg by oral route once a day and he is under follow-up with Hematology department for 6 months without recurrence or relapse. Written informed consent was acquired from the patient for presentation of this case report. DiscussionChronic lymphocytic leukemia (CLL) is the most common type of leukemia seen in adults and characterized by accumulation of B cells in lymphatic system for instance lymph nodes, spleen and other lymphoid organs [1,2]. Spleen and lymph nodes are frequently affected for patients with CLL; however head and neck involvement is uncommon. Regarding paranasal sinus involvement, CLL patients are prone to rhinosinusitis due to immunosuppression, 25-50 % of patients die due to paranasal sinus or urinary tract infections [2]. Gunel et al. reported 20 patients with CLL having rhinitis symptoms. Maxillary sinus was the most affected paranasal sinus with the inflammatory process, however none of their cases had paranasal sinus mucosa leukemic infiltration. Paranasal sinus leukemic involvement by CLL may be seen solitary or with lacrimal sac swelling as well as with orbital complication. [4,5] Lower airways such as bronchial mucosa may also be involved by tumor cells at the same time of paranasal sinus involvement. [6] With the available previous literature and our case; we can say that paranasal sinus involvement can be seen in two ways in CLL patients; inflammatory infiltration (rhinosinusitis) and leukemic infiltration. Leukemic infiltration may also cause secondary post-obstructive rhinosinusitis with mucosal edema [3]. Maxillary sinus is the most involved sinus in both leukemic and inflammatory infiltrations (Table 1) [2]. As for our case, there was also leukemic infiltration of the paranasal sinuses in the pathological specimens and MRCNS was cultured in the tissue biopsies as a sign of secondary post-obstructive rhinosinusitis.
Leukemic infiltration of the paranasal sinuses can be the initial finding for patients with CLL or can be seen years after CLL treatment as a sign of the relapsing disease (Table 1). Since the symptoms of leukemic paranasal sinus infiltration mimic inflammatory infiltration, CLL patients having rhinitis symptoms (nasal obstruction, nasal or postnasal discharge) unrefractory to medical treatment should be evaluated thoroughly. Paranasal sinus biopsies should be obtained after computerized tomography findings to make the diagnosis of leukemic infiltration and to rule out a secondary malignancy other than CLL due to immunocompromised state of the patient. Secondly, CLL patients having Ibrutinib (Imbruvica; Johnson&Johnson Medical, Istanbul, Turkey) treatment and rhinitis symptoms as in our case must be examined meticulously. Ibrutinib is an irreversible inhibitor of Bruton’s tyrosine kinase which is an important molecule for B-cell signaling system. It is widely used for the treatment of CLL patients. Patients with CLL undergoing Ibrutinib treatment may have affinity to invasive fungal infections even in the non-neutropenic state [7,8]. Eschar or mucosal necrosis in the endoscopic examination may be the signs of rhino-cerebral invasive fungal infections in these cases. There was no eschar tissue or mucosal necrosis in the initial examination of our patient, and there was no sign of invasive fungal infection in the pathological and microbiological evaluation of the patient. There is no globally accepted treatment algorithm for patients with CLL involving the paranasal sinuses. For patients with sole paranasal sinus involvement, surgical decompression of the sinuses may improve the patient clinically [3,4,8,9]. Such patients may be followed-up without chemotherapy if the patient remains asymptomatic with stable peripheral blood counts [5]. For patients with chemotherapy history, additional chemotherapy regimens or immunomodulatory treatment with Ibrutinib may be administered as a salvage treatment modality [3,6]. For our case, the patient had been already receiving Ibrutinib treatment. After endoscopic sinus surgery, he continued receiving Ibrutinib medication without chemotherapy since he had stable blood counts and did not have any recurrence or relapse. With previous reports and our case, we can say that each CLL patient with paranasal involvement must be individualized and treatment regimen must be chosen according to the clinical situation of the patient. In conclusion, CLL patients have a tendency to paranasal sinus infections. Although most cases having rhinitis symptoms are diagnosed as rhinosinusitis, paranasal sinus leukemic infiltration may be encountered rarely. Endoscopic sinus surgery with exploring the involved paranasal sinuses is mandatory for cases refractory to medical treatment. Both paranasal sinus biopsies and tissue culture specimens must be obtained during surgery to diagnose the leukemic infiltration and post-obstructive rhinosinusitis. Each CLL patient with paranasal sinus involvement must be individualized for treatment. Patients without additional symptoms and stable blood counts may be followed-up without chemotherapy regimen. Main Points
References
|
|||||
| Keywords : KLL , Paranazal Sinüs , Kronik Lenfositik Lösemi | |||||
|