|
|||||||||||||||
AbstractChordomas which originate from embryonic notochordal remnants are uncommon and slow-growing tumors of axial skeleton. Chordomas account for less than 1% of central nervous system tumors in spite of the fact that they present intracranially in approximately one third of all cases. The vast majority of intracranial chordomas are located in the skull base, especially around the clivus. On the other hand, these tumors are quite rare in the sellar region. Herein, we present a 45-year-old man applied with complaint of headache and droopy right eyelid. On magnetic resonance imaging, a sellar mass sized 34x30x27 mm that resembles to pituitary macroadenoma was detected. Endoscopic transnasal transsphenoidal surgery was performed to relieve the compressive symptoms. However, the mass could be partially removed by surgery because of its tight adhesion to the surrounding tissues. In histopathological examination, chordoma was diagnosed contrary to our expectation of other common tumors of the sellar area such as pituitary macroadenoma, craniopharyngioma, and meningioma. Thereupon, the patient was referred to a tertiary hospital to be evaluated in terms of external beam therapy. Most of sellar chordomas are prone to local recurrence; therefore radiotherapy should be given as adjuvant therapy if the mass could not be totally removed.IntroductionChordomas are malignant bone tumors which derive from embryonic remnants of the notochord. These rare tumors can emerge anywhere along the skeletal neuroaxis, however, mainly involved regions are midline structures such as the sacrum, the skull base, and the spine with each almost equal incidence to each other. Chordomas constitute approximately 1% of all malignant tumors of the bone and 0.2% of all intracranial tumors [1]. It has been reported that they usually occur in the fifth to sixth decades with a slight male preponderance. Chordomas located in the skull base may be noticed relatively younger ages, its cause is presumably that intracranial tumors lead to early signs including headache and cranial nerve palsies. Almost all of intracranial chordomas present around the clivus, on the other hand the sellar region is infrequently involved. Sellar chordomas may arise from parasellar and suprasellar bones. As a matter of course, these tumors may mimic pituitary adenomas. Furthermore, various hormonal problems and visual defects may also develop due to compression of the pituitary gland and optic chiasm by the mass, respectively. Chordomas extending to parasellar area may cause oculomotor nerve palsy while skull base chordomas are associated with abducens nerve palsy [2]. Despite their slow-growth feature, chordomas are characterized with erosion of the bone and infiltration to the adjacent soft tissues. Therefore, gross-total resection is quite difficult as well as they tend to local recurrence compared to distant metastasis. The definitive diagnosis is often required histological examination because of these tumors have neither clinical nor radiological specific features. We aimed to report this case with sellar mass, which is thought to have a pituitary macroadenoma, but was diagnosed with chordoma by endoscopic transnasal transsphenoidal surgery. Case ReportA 45-year-old male patient had recourse to Neurosurgery department of our hospital with complaints of headache and droopy right eyelid. The patient stated that he suffered from headache for a few months but the droopy right eyelid has gradually developed in about 1 week. He had not any known illness as well as his family history was unremarkable. On physical examination, there was no pathological finding except ptosis of the right eye that is suggesting the compression of oculomotor nerve. MRI of the brain showed a mass lesion which is 34x30x27 mm sized and completely occupies the sellar cavity (Figure 1).
The mass compressing optic chiasm on superior and extending to cavernous sinuses on both sides was presumed as a pituitary macroadenoma at first view. Cranial CT revealed that sellar mass has internal calcification areas (Figure 2),
additionally the mass had prolapsed into sphenoid sinus due to destruction of the sellar floor. All the laboratory examinations including pituitary hormone tests were normal. The possibility of pituitary-dependent Cushing’s disease was also excluded preoperatively via 1 mg dexamethasone suppression test. Nonfunctioning pituitary macroadenoma, craniopharyngioma, and meningioma were primarily suspected in the light of preliminary findings. We thereupon decided to surgery both to achieve the final diagnosis and to provide the decompression of oculomotor nerve. Endoscopic transnasal transsphenoidal surgery as a minimal invasive technique was performed by neurosurgeon-otolaryngologist collaboration (Figure 3).
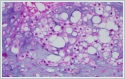
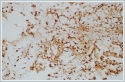
The operation was completed without any complications, but the mass could be partially removed because of its tight adhesion to the surrounding tissues. The postoperative course was uneventful including the pituitary functions. His ptosis also improved markedly within a few days following the operation. Histopathological examination unexpectedly revealed that the lesion consisted of the tumor cells with vacuolated cytoplasm which are also called physaliphorous (bubbly) cells associated with chordoma in a background of myxoid matrix (Figure 4).
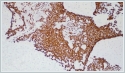
Immunohistochemical analysis disclosed that the neoplastic cells were stained positively for protein S-100, epithelial membrane antigen, pancytokeratin and vimentin but negatively for synaptophysin, FSH, LH, ACTH, GH, and TSH (Figure 5).
Ki67 proliferation index was 10%. As a result of all these studies the definitive diagnosis of chordoma was established, thereafter the patient was referred to a tertiary hospital to be evaluated in point of external beam therapy as an adjunctive treatment option. DiscussionChordomas are relatively slow growing and locally invasive bone tumors that are associated with dysembryogenesis. Sellar chordomas can be considered as a rare subgroup of the skull base chordomas which constitute with 35% of all chordomas. These tumors usually cause to headache or signs of cranial nerve compression [3]. Diplopia, visual blurring, ptosis, and ophthalmoplegia due to compression of oculomotor and abducens nerves may be seen. Other tumors setting at the same location such as pituitary adenoma, craniopharyngioma, meningioma, and chondrosarcoma should be considered in differential diagnosis of sellar chordomas. CT scan mostly shows the calcified hyperdense mass and lytic lesions related to local bone destruction. MRI is the most favored radiological method about the evaluation of soft tissue involvement. The characteristic histopathological feature of chordomas is physaliphorous cells that are the tumor cells including variably sized cytoplasmic vacuoles in a ground of mucinous extracellular matrix. Immunohistochemically, chordomas display the reactivity to cytokeratins, vimentin, epithelial membrane antigen, and protein S-100. Brachyury, a novel diagnostic biomarker for chordomas, is a transcription factor which plays a crucial regulatory role in embryogenetic differentiation of the notochord. However, brachyury could not be analyzed in our case due to technical inability. Surgical excision as broad as possible is the principal step to treat a sellar chordoma. On the other hand, it must also be paid attention to safety of vital neurovascular structures in the parasellar area. Transsphenoidal approach which is a minimally invasive procedure to remove the sellar tumors is the outstanding surgical technique, particularly in recent years. Compared with the traditional technique, the endoscopic transnasal approach is associated with a shorter operative time, shorter hospitalization time and without any complications like bleeding, leakage of cerebrospinal fluid, menengitis and other intracranial complications. However, en bloc resection of chordomas is highly difficult because of locally infiltrative behavior of these tumors. Therefore, adjuvant radiotherapy has been suggested to warrant the optimal treatment by most authors [4,5]. The mass was strictly adhered to the surrounding tissues in our case too that is why an aggressive resection could not be performed. The patient was referred to radiotherapy as soon as chordoma is diagnosed histopathologically. Adjuvant radiotherapy whether to prolong survival in case with gross-total resection of skull base chordomas is controversial, but it is strongly recommended in the patients with incomplete resection. Photon-based radiation therapies (Fractionated external beam therapy, Gamma Knife, Cyberknife, Intensity-modulated radiotherapy), proton beam therapy, and carbon ion radiotherapy may be given as adjunctive therapy. However, it has also been reported that there is no difference between the modalities of adjuvant radiotherapy in terms of overall survival of the patients with skull base chordomas [6]. Conventional cytotoxic chemotherapies are not effective in the treatment of chordomas. Therefore, it should be aimed to achieve cytoreduction with complete tumor resection, if possible, and adjuvant radiotherapy if necessary. Additionally, molecular targeted therapeutic agents such as imatinib, afatinib, rapamycin, and the combination of bevacizumab and erlotinib might be useful in the treatment of some patients with chordoma [7-10]. It seems possible that brachyury may also be a potential target of the treatment of chordoma in the near future. Consequently, sellar chordoma is a rare clinical entity and it may be simulated to pituitary adenoma in first evaluation. Therefore, it should be taken into account in the differential diagnosis of sellar tumors and should be adopted a multidisciplinary approach in its management. Abbreviation list: MRI (magnetic resonance imaging), CT (computed tomography) FSH (follicle-stimulating hormone), LH (luteinizing hormone), ACTH (adrenocorticotropic hormone), GH (growth hormone), TSH (thyroid-stimulating hormone). References
|
|||||||||||||||
| Keywords : Kordoma , Endoskopik Transnazal Cerrahi , Sellar Kitle. | |||||||||||||||
|