|
|||||||
Turkish abstractÖlümcül orta hat granülomu olarak da bilinen nazal tip doğal katil (NK) /T hücreli lenfoma oldukça agresif seyirlidir. Hastanın sağkalımını uzatmak için yüksek derecede şüphe ve erken tanı gereklidir. Nüks oranı yüksek ve tedaviye yanıt düşüktür. 63 yaşındaki erkek hasta kliniğimize 2 yıldır sağ burun tıkanıklığı, burun kanaması ve sağ gözde diplopi şikayetleri ile başvurdu. Fizik muayenede sağ nazal kaviteyi tam obstürkte eden kolay kanayan ülsere kitle görüldü. Paranazal sinüs bilgisayarlı tomografisi (BT) ve kontrastlı yüz manyetik rezonans görüntüleme (MRG) tetkiklerinde sağ maksiller, etmoid, frontal sinüsleri, nazal pasaj sağ yarısını dolduran kitlenin histopatolojik tanısı ekstranodal nazal tip NK/T hücreli lenfoma olarak raporlandı. Bu makalede NK/T hücreli lenfoma olgusu tanı, tedavi süreci, radyolojik, klinik ve immünohistokimyasal bulguları ile birlikte güncel literatür eşliğinde sunulmuştur.IntroductionNasal type NK / T-cell lymphoma (NKTL) is characterized by necrotizing mucosal lesions of the facial midline region and upper aerodigastric system destroying bone and cartilage. It causes severe functional and cosmetic deformity [1,2]. It is a rare disease in the nose and paranasal sinuses. Due to its very aggressive course and poor prognosis, early diagnosis and treatment are very important in d sease management [3]. In this case report, a patient diagnosed with NK / T cell lymphoma is presented clinically and histopathologically in the light of the current literature. Case Report
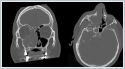
There was no palpable lymph node in the neck. Paranasal sinus tomography revealed a mass leyson that filled the right maxillary, ethmoid, frontal sinuses, and right half of the nasal passage (Figure 2).
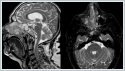
It was interpreted that there is a central hypointense lesion with peripheral enhancement, which is observed as T1W hypointense in the same localizations and iso-heterogeneous hyperintense in T2W sequences in contrast-enhanced facial MRI imaging (Figure 3).
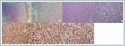
As a result of the consultation of ocular diseases, baseline diabetic retinopathy was observed. Multiple punch biopsies were taken from the mass in the right nasal passage under sedation. In the biopsy material sent, coagulative necrosis, acute and chronic inflammation in focal areas and an atypical lymphoid cell infiltration with small / large diameter nuclei, including atypical mitoses, were observed. Hyperplasia and ulceration were observed in the squamous epithelium infiltrated by atypical lymphoid cells in some areas. In the immunohistochemical study, CD56 diffuse (+), CD3 diffuse (+), CD8 (+), CD5 (+), CD20 (-) were stained (Figure 4).
Pankeratin was (+) stained in the epithelium and no staining was detected in the infiltration area. The case was reported as Extranodal Nasal type NK- / T-Cell Lymphoma with current findings. Positron Emission Tomography (PET) CT was performed for staging purposes and bone marrow biopsy was performed. Distant metastasis was not observed. A non-hodgkin lymphoma (NHL) panel was studied by the hematology, using the fluorescent in situ hybridization (FISH) method. TP53 (17p 13.1 deletion), MYC / CEP8 t (8; 14), BCL2 t (14; 18), CCND1 t (11; 14) translocations were found to be negative. Combined chemoradiotherapy was planned simultaneously with the diagnosis of stage 1 extranodal nasal type NKTL. He received 4 doses of DeVIC (dexometasone, etoposide, ifosfamide, carboplatin) and 28 cures radiotherapy. There was no recurrence in the control MRI, PET CT, CT and physical examinations of the patient, who was in the 9th month of the follow-up. DiscussionThe term "deadly midline granuloma" was first described in history by McBride in 1897. It is an idiopathic ulceration process that causes severe destruction of the nose and oral cavity in the central facial region. In 1922, Stewart published 10 cases of chronic destruction of the mid-face region as Stewart's syndrome or Stewart's Granuloma. In 1949 Williams popularized the term LMG as inflammatory midline destructive lesions of unknown etiology. The terms "Fatal midline granuloma" or "Granuloma Gangrenescens" have been used for the aggressive and mortal disease that includes severely necrotic granulomas [4]. In the past, terms such as polymorphic reticulosis, malignant midline reticulosis have also been used for this disease [5]. NKTL should be differentiated from progressive ulcerative disorders of midline facial tissues such as sarcoidosis, syphilis, Wegener granulomatosis, tuberculosis, cocaine use, polymorphoreticulosis, and septal carcinoma [4]. Lymphomas of the nasopharynx and nasal region are usually NHL. It can transform into NK / T cell type, peripheral T cell type or B cell type. The most common type in the nasal type region are extranodal NK / T cell lymphomas [5]. NK / T cell lymphoma is most common in 40-50 years of age. It is associated with a distinct geographic and ethnic region that particularly affects Latin American and Asian societies. Although association with Epstein Barr Virus (EBV) and genetic predisposition (p53 and c-kit gene mutations) have been reported, its pathogenesis is not clearly known [6]. The male / female ratio ranges from 8: 1 to 2: 1 [7]. Our patient was a 63-year-old male. The disease can be seen in three stages: prodromal stage, active stage, and terminal stage. In the terminal stage, progressive destruction extending from the nasal cavity, palate, upper lip to the aerodigastric system, and large destructive lesions in the mid-face line are seen. It can cause metastasis and death [1]. In the early stage of the disease, nonspecific symptoms such as nasal congestion, runny nose and nosebleeds are seen. Rarely, systemic findings such as fever, night sweats, weight loss and anemia can be seen. On physical examination, septal perforation, widespread ulceration in the septum and inferior concha, and widespread necrosis with destruction of bone and cartilages in later stages are observed. Regional lymphadenopathy is defined in 15-25% of cases [6]. Our patient had complaints of nasal congestion and bleeding. Double vision and vision loss had recently started. Physical examination revealed a bleeding ulcerated mass that obstructed the right nasal cavity. There was no palpable lymph node in the neck. In the early phase, clinical features may mimic chronic rhinosinusitis, and CT imaging may show a homogeneous lesion that is limited to the nasal cavity, without necrosis, without contrast, in these cases [3]. Angioinvasion and necrosis are always seen histopathologically. Plasma cells, polymorphonuclear neutrophils, reactive histiocytes with erythrophagocytosis, areas of coagulation necrosis without signs of vasculitis confirm the diagnosis. In immunohistochemical examination, T lymphocyte phenotype, negative surface CD3 and positive cytoplasmic CD2, CD3 and CD56 markers with cytotoxic markers (TIA-1 and granzyme B) are usually seen. EBV can be positive or negative [3,6]. In our patient coagulative necrosis in focal areas, acute and chronic inflammation together with variable cell size, small / large diameter nuclei, atypical lymphoid cell infiltration including atypical mitoses, hyperplasic changes in the surface squamous epithelium and ulceration were observed. It was CD3 (+), CD56 (+), CD5 (+), CD8 (+), CD20 (-). This disease is referred to as angiocentric lymphoma in the Revised European American Lymphoma (REAL) classification and as nasal type NK / T cell lymphoma in the World Health Organization European Organization for Cancer Research and Treatment (WHO-EORTC) classification [4]. Treatment is difficult and complex and depends on the stage of the disease. Planning should be done with hematologists and oncologists in a multidisciplinary manner. Since the disease is very rare, studies for standard treatment are still ongoing and a definitive treatment has not yet been defined. Some authors stated that surgical treatment is ineffective and may cause the lesions to deteriorate by allowing the disease to progress rapidly. Surgical treatment is limited to the purposes of biopsy, airway opening and debridement [6,7]. Surgery was performed for our patient for diagnostic purposes. Multiple punch biopsies were taken from the mass in the right nasal passage under sedation. Wang et al. reported that application of radiotherapy following chemotherapy increases progression-free survival [8]. Some centers use anthracycline-based combination chemotherapy followed by radiotherapy for patients under 60 years old, and anthracycline-free chemotherapy for older patients. Other authorities have reported remission rates reaching 40-80% with 52 Gray RT with 40-59% survive rates in the early stages. It has been reported that if chemotherapy fails, radiotherapy can improve prognosis. Immunotherapy may be the treatment of the future. Interferon, on the other hand, has not been shown to be effective. NK / T cell lymphoma has a poor prognosis, 5-year survival rates are between 10-45%, depending on the literature series [6]. We recommended 4 doses chemotherapy and 28 cures radiotherapy to our patient, and the follow-up process continues. Left untreated, septicemia has a very high mortality rate, reaching almost 100%, due to perforation of blood vessels or a brain abscess [5]. Consequently, a high degree of suspicion is absolutely necessary for the diagnosis of NK / T cell lymphomas, which are extremely rare. Accurate and early diagnosis can prolong survival. This disease should be kept in mind as a differential diagnosis in nonspecific nasal cavity lesions. Since the recurrence rates are high and their response to treatment is low, patients should be followed up regularly. References
Presented at42. Ulusal Türk Kulak Burun Boğaz Baş ve Boyun Cerrahi kongresinde poster olarak kabul edilmiştir. |
|||||||
| Keywords : NK/T hücreli lenfoma , ölümcül orta hat granülomu , baş boyun bölgesi | |||||||
|