|
|||
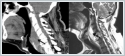
AbstractRetropharyngeal abscess (RA) is life-threatening disease if not diagnosed and treated timely and cause airway obstruction and asphyxiation. Even RA is not rarely observed, the management of RA still contains some contradictions. Here, we report and discuss RA management with three cases.IntroductionRetropharyngeal abscess (RA) is a deep neck infection mostly seen in pediatric population. Even it is unusual in adults, it can be dangerous and life-threatening if not diagnosed and treated timely and cause airway obstruction and asphyxiation [1-4]. RA mostly occurs following an upper respiratory tract infection. Other common causes in adult populations are cervical trauma and tuberculosis. Even RA is not rare, management of RA still contains some contradictions. Our aim is to discuss RA management with three cases. Case ReportCase 1: A-59-year-old female patient presented to our clinic with dyspnea and reduced neck movement. Patient had a history of upper airway infection one month ago. Physical and endoscopic examination revealed a huge posterior mass starting from at the level of tongue base extending to the level of larynx. There was no fever and acute phase reactants were in normal range. Patient had a magnetic resonance imaging (MRI) and computed tomography (CT) of the neck in another hospital which was revealed an abscess with approximately 25x19x11mm (Figure 1) and some changes in cervical vertebrae.
After hospital admission, intravenous (iv) systemic antibiotics with ampicillin-sulbactam (4x1.5gr) was administered. Surgical drainage in operational settings was performed in Trendelenburg position. A thick pus was drained and multiple samples were obtained for microbiological examination including samples for tuberculosis test. However, there was no growth in cultures and no sign of tuberculosis. Even it is an uncommon cause, microbiological test for tularemia was sent and the result was positive. Patient was administered intramuscular streptomycin sulfate (1000mg/daily) for 12 days followed by oral tetracycline (100mg, 2 times per day). She was symptom free in six months follow-up. Case 2: A-33-year-old male presented to our clinic with generalized neck swelling, difficulties with swallowing, reduced neck movement and severe dyspnea. Patient had a history of upper airway infection 1 week ago. He used oral amoxicillin clavulanate (1000mg, 2 times per day) for 5 days followed by intramuscular ceftriaxone (1 gr, 2 times daily) for 2 days. However, symptoms increased despite the continuous antibiotic therapy. The patient had been recurring emergency service admission to many different hospitals. He had no other known medical disease. Physical examination revealed a generalized neck swelling, severe dyspnea and flexible endoscopic examination revealed a retropharyngeal abscess causing airway obstruction. Patient had normal acute phase reactants. Neck CT demonstrated 57x28mm abscess formation in retropharyngeal area extending to larynx and causing airway obstruction (Figure 2).
Direct laryngoscopy and drainage of abscess were performed under general anesthesia. The abscess drained via a vertical incision at the level of epiglottis and multiple samples for culture were obtained. Results showed any microorganism growth in culture and no sign of tuberculosis in PCR test. Patient was not extubated after the surgery to be sure whether the airway was secured as the larynx was edematous during difficult intubation and transported to intensive care unit (ICU). He was extubated 2 days after ICU follow-up. After following for 14 days with iv piperacillin -tazobactam (4,5gr, three times per day), he was discharged. During follow up, control CT scan showed no abscess formation in neck (Figure 3). Case 3: A-44-year-old male presented to our clinic with a dysphagia for 10 days which was worsened in the last couple of days. There was no history of other symptoms including fever, coughing or dyspnea and any other medical disease. Physical examination revealed palpable lymph nodes and retropharyngeal swelling at the level of epiglottis was detected in flexible endoscopic examination. Neck ultrasound (USG) showed multiple LN in size 15 mm bilaterally and a retropharyngeal left sided 60x18x31mm and right sided 21x11mm fluid collection. A neck CT was performed to detect the exact level of the abscess and for planning the drainage pathway. It demonstrated an abscess formation between C2 and C7 vertebrae with a longitudinal size of 6,5 cm which compressed the trachea to anterior and shifted it to the left side (Figure 3).
All acute phase reactants were in normal range. A surgical drainage was decisioned. Suspension laryngoscopy was performed and a clear view of the area achieved with a 0-degree rigid endoscope. During the operation, a vertical retropharyngeal incision at the level of epiglottis were performed, muscles were incised and separated. The abscess wall was opened and drained with multiple biopsies. Culture materials including tuberculosis were obtained. After control of bleeding, a nasogastric tube was inserted and patient extubated safely. Patient was administered i.v. piperacillin -tazobactam (4,5g, three times per day) for 3 days followed by oral ampicillin- sulbactam (1gr, two times per day) and ciprofloxacin (500mg, two times per day) treatment for 14 days. Patient started to oral intake on third day and was discharged. All culture results were normal including tuberculosis PCR test. Histopathology was reported as chronic inflammatory findings. At the follow up, a flexible endoscopic examination in two weeks showed complete resolution of abscess with a well healed mucosa (Figure 3). DiscussionA good anatomical knowledge of the retropharyngeal space is crucial to understand this life-threatening disease. Buccopharyngeal fascia, alar fascia and prevertebral fascia are three fascial layers in deep neck from anterior to posterior. RA grows between buccopharyngeal and alar facia called retropharyngeal space. Retropharyngeal space extends from skull base to posterior mediastinum and contains multiple lymph nodes. These nodes usually get atrophy after the age of five. Many patients with retropharyngeal abscess had a history of upper respiratory tract infection, which may cause lymphadenitis in retropharyngeal space and caused abscess formation [4,5]. As mentioned before, abscess due to infections are relatively rare in adults and mostly observed in young children. In adult cases, the most common reason is trauma to the retro pharynx. There are also some case reports in literature with spontaneous RA or abscess with an unknown etiology [6,7,8]. Tuberculosis must be remembered in adult cases with retropharyngeal abscess, in spite it is not common cause [1,2,7-9]. RA are polymicrobial infections including upper airway anaerobic pathogens; Group A beta-hemolytic streptococcus, Haemophilus and Fusobacterium species [1,3]. In our case series, second case had a history of an upper airway infection before abscess formation which we decided as a possible cause despite no evidence of microorganism. In first case with a history of airway infection and without having a history of contact with the microorganism Francisella tularensis were detected. In adult patients, it is possible to have different unusual etiologies that cause RA and physician should be aware of different microbiological etiologies that may change the medical treatment modalities. It is possible not to detect any microorganism as in our second and third case and wide-broad spectrum antibiotics were needed to treat the RA after surgical drainage. Patients may present with dysphagia, neck stiffness, neck swelling and respiratory distress. Patients are usually febrile and ill looking. Severe dysphagia may occur and patients may refuse to oral intake of any food or fluid. However, this are mostly observed in patients with acute infections. Patients with cold abscess may not have any symptom. In our cases, dyspnea, dysphagia, neck swelling and limited neck movements were the main symptoms of RA and none of the patients had a fever or ill looking. Unknown etiologies are more frequent in adults as in second and third case. It is possible to have it presented with not specified symptoms and a high level of suspicion with a full otorhinolaryngologic examination is mandatory for a precise diagnosis in some cases as our third case. Examination of patients with retropharyngeal abscess must be done carefully and should be performed preferably in Trendelenburg position since there is a risk of rupture of abscess. This may prevent aspiration and asphyxiation if the abscess rupture occurs [5-7,9,10]. Blood counts, infection parameters such as C-reactive protein, sedimentation, and cultures should be checked. However, it is remembered that they may be in normal range in cold abscess as in all of our cases. Neck CT may be performed for assessment of extension. CT imaging helps clinicians to determine upper airway patency and need for an emergency intervention to achieve a secure airway. Securing airway with emergency tracheotomy is crucial before any imaging if RA causes serious airway obstruction and no emergency tracheotomy to secure airway was needed in our cases. All patients with a RA needs hospital admission to be able to perform timely intervention. The treatment also requires systemic antibiotic therapy covering upper respiratory tract pathogens. In conclusion, retropharyngeal abscess may occur as an insidious infection in adults and can be life threating if not detected and treated timely. Acute phase reactants and microbiological results may not be reliable tools in cases for diagnostic purposes. Only history or only physical examination may not be helpful to diagnose RA and to detect the etiology. Drainage of the abscess must be done in all cases however, in terms of medical treatment, a tailored approach will have more benefits and prevents excessive use of antibiotics. References
|
|||
| Keywords : Retrofaringeal apse , hava yolu , tıkanıklık , drenaj | |||
|