|
|||||||||||
AbstractA 77-year-old woman with metastatic renal cell carcinoma to the thyroid and parotid gland was presented in this study. Metastatic neoplasms of the head and neck region are so rare that they have been usually reported as case reports. The present case is the a patient admit because of facial paralysis who had both of the thyroid and parotid gland metastasis of renal cell carcinoma. The clinical presentation, radiologic and pathologic investigations, and the treatment of patient with surgery were discussed.IntroductionThree percent of cancers in adults involve the kidneys, 80% of these being clear-cell carcinoma. Evolution is unpredictable: either revealed by multiple metastasis, or dormant over a long period before recurrence. Metastasis may involve any organ, which complicates diagnosis. Six percent of atypical metastasis locations are head and neck, and notably at three sites: thyroid, sinus and parotid gland [1] . An extremely rare case of a metastatic renal cell carcinoma(RCC) to both of the thyroid and parotid gland with facial paralysis was presented in this study. To our knowledge, it is the first case reported in the literature. Case ReportN.H. is a 77 year old female presented right neck mass extending to right parotid and thyroid glands and with a history of RCC of both kidneys, which had been totally excised at the left side and partially at the right side 3 years ago. The mass had grown rapidly over the previous 12 months. She had right peripheral facial paralysis for 5 months and right hemi-cranial pain (Figure 1).
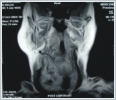
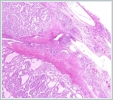
Fine needle aspiration biopsies(FNAB) taken 3 times were reported as insufficient specimen with full-filled blood cell. Magnetic resonance imaging (MRI) revealed 55x51 mm hyper vascular mass, probably a malignant tumor which was originated from the deep and superficial lobe of parotid gland, approximately 1 cm lymphadenopathy in the right side of the neck, partial thrombus in the right internal juguler vein and nodular goiter of the right thyroid (Figure 2, 3). Another imaging method was not used.
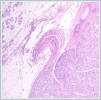
However, the specimen was quite bloody and suspicion remained high for a metastatic lesion given the patient’s history of renal cell carcinoma. On Novenber 2004 the patient underwent right total parotidectomy, radical neck dissection and hemithyroidectomy with isthmusectomy. Buccal and zygomatic branches of the facial nerve were scarified because of the tumor invasion. Permanent pathologic specimen revealed metastatic renal cell carcinoma, clear cell type (Figure 4, 5).
DiscussionRenal cell carcinoma is infamous for its unpredictable behavior and metastatic potential. Although the most common sites for RCC metastasis are the lung, lymph nodes, bone, liver, adrenal and brain, this neoplasm may involve any organ including the both of and thyroid parotid as an unusual metastatic site [2]. In a study by Bernicker et al of 65 patients with RCC metastasis to the head and neck, none of the patients presented with parotid metastasis. The first case of RCC metastatic to the parotid gland was published by Patey et al in 1965 [3]. From the literature over the past 50 years, we identified an additional 35 reported cases of metastatic RCC to the parotid [4]. Renal cell carcinoma metastases to the thyroid gland account for 12 to 34% of all secondary thyroid tumors. Metastatic thyroid tumors may represent the first manifestation of RCC or a synchronous or metachronous metastasis of a known RCC. Metastases usually appear as metachronous lesions, often several years after nephrectomy [5]. Although uncommon, more than 150 cases of clinically recognized metastatic renal cell carcinoma to the thyroid have been reported in the literature [6]. In patients presenting with parotid bulk and rarely facial paralysis, unless one maintains a high index of suspicion, the unsuspected disease may be completely overlooked. Radiological findings are indistinguishable from those of a primary cancer. Parotid ultrasonography reveals a heterogeneous lesion and head and neck computed tomography(CT) with contrast findings are not specific. Some authors confirm the diagnosis using FNAB although false-positive and false-negative cases have been reported. Even when FNAB can not differentiate between primary parotid cancer and metastases from other primary lesions, it provides important information for management of the patient. Especially, clear cell tumours present a diagnostic challenge to the pathologist. A considerable array of diagnostic alternatives exists [2,7,8]. The use of periodic-acid Shiff (PAS) with enzymes, such as diastase and mucin stains, is helpful in distinguishing primary salivary gland tumours which may have clear cell areas, such as acinic cell and mucoepidermoid carcinomas from RCC. Generally, RCC contains glycogen, making it PAS positive and diastase negative; on the other hand, acinic cell carcinoma and mucoepidermoid carcinoma are revealed as PAS positive and contain diastase-resistant material . In the case of clear cell thyroid gland tumours, the use of thyroglobulin immunohistochemistry can help to distinguish from metastatic RCC [9,10]. The mechanism by which a renal cell carcinoma reaches the parotid gland is probably the haematogeneous spread. In fact, renal cell carcinomas are hypervascular tumours associated with multiple arteriovenous shunt. Considering the fact that kidneys receive 25% of circulating blood volume, renal cell carcinoma has a high haematogeneous spreading potential[2, 7]. On the basis of the extension of the disease, treatment is consistently different. Treatment of diffuse metastatic disease is a combination of chemotherapy, immunotherapy, hormone therapy and radiation therapy, but the results are dismal. On the other hand, it is well known that management for clinically solitary metastasis is aggressive surgical resection. In patients with a solitary metastasis amenable to surgical resection the five-year survival rate was 53% . Solitary parotid metastasis and a long interval are favourable prognostic factors [7,11]. Metastatic disease should always be considered in the differential diagnosis for patients who present with salivary or thyroid gland swelling and very rarely facial paralysis with a previous history of renal cell carcinoma. Standard diagnostic measures such as FNA may not yield a definitive diagnosis and patients must be counseled accordingly. Based on our literature review, this case represents the longest duration for recurrence of RCC metastatic to the parotid gland. If metastatic disease is confined to these glands only, prompt surgical excision can be curative. References
|
|||||||||||
| Keywords : Renal , Karsinom , Metastaz , Tiroid , Parotis , Fasyal , Paralizi | |||||||||||
|