|
|||||||
AbstractThe increase in the incidence of squamous cell carcinoma in the lateral part of the tongue in young, non-smoking and female individuals in recent years and the fact that HPV and other viral factors remain etiologically unclear in these cancers indicate that different etiopathologies should be investigated in lateral SCC of the tongue. The case is the first reported case of OSCC after orthodontic treatment in a low-risk young female patient.IntroductionOral squamous cell carcinoma (OSCC) is a malignant tumor that begins with dysplasia of the multilayered squamous epithelium lining the oral cavity and develops when neoplastic cells cross the basement membrane and invade the subepithelial space. It accounts for more than 90% of cancers of the oral cavity. Various risk factors may lead to OSCC formation by causing mutation accumulation leading to significant neoplastic transformation in the long term. In this sense, advanced age has a central role in allowing the accumulation of genetic alterations to promote carcinogenesis. The strongest risk factors for OSCC are smoking and alcohol [1,2]. However, the most important etiological factors are Human Papilloma Virus (HPV), nutritional deficiencies, tobacco chewing and gene mutations. Chronic trauma of the oral mucosa is also cited as a risk factor. Defective teeth (incorrectly positioned, sharp or rough surfaces due to decay or fractures), unsuitable dentures (sharp or rough surfaces, stability problems) and parafunctional habits (e.g. biting or sucking the oral mucosa, tongue thrusting), acting individually or together, can all be responsible for this mechanical trauma. Intraoral chronic trauma can create lesions in a healthy mucosa or exacerbate previous oral diseases [3]. Only 0.6% (<21) of all OSCC cases affect young people, and the vast majority of cases have been detected in the tongue. In recent studies, an increasing tendency for tongue cancer has been found in young people compared to adults. Most of this increase has been observed in white women who do not smoke or drink [4]. The case is the first reported case of OSCC after orthodontic treatment in a low-risk young female patient. Case ReportA 21-year-old woman presented to the clinic with a rapidly growing ulceration in the medial-lateral region of her tongue which she noticed 3 months ago (Figure 1). It was learned that she did not have any systemic disease, did not smoke and rarely consumed alcohol.
In the anamnesis, the patient stated that he had been undergoing orthodontic treatment for 1.5 years and that the area was exposed to trauma during treatment. The patient's oral hygiene was described as good. On intraoral examination, the lesion was exophytic, painless, firm on palpation and covered with red and white ulcerated tissue. Ultrasound images showed increased basal blood flow at the base of the lesion (Figure 2). In addition, a lymphadenopathy with a normal blood supply pattern was observed in the left submandibular region (Figure 3).
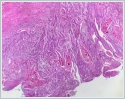
In this case, an approximately 1 cm tumor with a depth of 2.5 cm was removed by excisional biopsy. After excisional biopsy, the lesion was histopathologically diagnosed as moderately differentiated squamous cell carcinoma (Figure 4). Since the surgical margins were positive, the lesion was excised in the ENT clinic by extending the lesion grades 1 cm in each direction, right supraomohyoid neck dissection was performed and the defect was reconstructed with split thickness skin graft (STSG).
The 2[nd] biopsy result of the patient was defined as a material with high degree of dysplasia, no residual invasive tumor and intact surgical margins. No lymph node metastasis was detected. Chemotherapy and radiotherapy were not administered to the patient. At the end of the 1[st] year, the appearance of the tongue area was healthy, tongue movements and function were complete (Figure 5). Facial nerve function was complete at the 1[st] year after dissection (Figure 6). DiscussionThe most prominent patient profile in OSCC is that of male smokers aged 40-60 years. In recent years, HPVs constitute an important etiologic group of these cancers. HPV has been detected in 80% of OSCCs especially in the oropharynx, but HPV remains unclear for OSCCs occurring on the tongue [5,6,7]. In 2015, JS poling et al. evaluated the role of HPV in lateral SCC of the tongue and reported that HPV was not detected in most cases and HPV was not an important risk factor in SCC of the lateral tongue [7]. Furthermore, recent epidemiologic studies have not consistently isolated specific viral genetic material in tongue SCCs [8,9]. The increase in the incidence of squamous cell carcinoma in the lateral part of the tongue in young, non-smoking and female individuals in recent years and the fact that HPV and other viral factors remain etiologically unclear in these cancers indicate that different etiopathologies should be investigated in lateral SCC of the tongue. Another risk factor for OSCCs in low-risk young patients is mutations. However, in a study conducted in 2008, it was stated that mutations alone are not sufficient to produce cancer and that they need one or more promoters [10]. In epidemiologic models, the effect of promoters on carcinogenesis appears to be more important than the initiating factor. Studies suggest that intraoral chronic trauma plays a role at least as a promoter in carcinogenesis initiated by another carcinogen [11,12,13]. In this case report, we presented how mucosal damage caused by orthodontic treatment can lead to SCC in a low-risk patient. Crooked teeth and dentures have recently been identified as risk factors for OSCC. It is known that denture wearers are more likely to have oral mucosal lesions than non-denture wearers and that these oral mucosal lesions can develop into malignancies in the oral cavity. There are studies suggesting that not only trauma but also electrical effects of denture metals in the mouth are important factors in the development of squamous cell carcinoma of the tongue [14]. On the other hand, oral SCC tumor formation is known to depend not only on the type, duration and extent of exposure to a particular carcinogen, but also on the genetic susceptibility of the individual. In this case, the young age of the patient may have masked a possible genetic risk factor. Considering all these studies and literature information, concluded that oral soft tissue and radiologic examination should be performed more carefully in young and low-risk patients undergoing orthodontic treatment, and biopsy should be performed in suspicious lesions regardless of smoking and age. During this process, sores in the mouth, aphthae caused by stress due to nutritional deficiencies and the difficulty of treatment are considered normal, which may make it difficult to recognize these lesions. Since one of the most important factors in the cancer method is early diagnosis, it is very important that dentists are aware of this issue. In young, low-risk patients with OSCC, a comprehensive treatment is recommended as the etiopathology is not fully established. Considering the life function and age of the patients, it is recommended to avoid aggressive treatment, follow-up for recurrence and investigation of genetic factors [3]. ConclusionFurther studies are needed to identify more specific etiopathological risk factors associated with oral SCC in pediatric, adolescent and young patients. Informed ConsentPrior to the examination, informed consent is obtained from each patient at the Ankara University Faculty of DentistryReferences
|
|||||||
| Keywords : skuamöz hücreli karsinom , dil , kadın | |||||||
|