|
|||||||||||
AbstractNasopharyngeal carcinoma is an epithelial neoplasm that originates from the mucosa of the nasopharynx, it is most commonly observed in Rosenmüller fossa. The primary treatment is radiotherapy. Early and late toxicities associated with radiotherapy are present in head and neck cancer. Acute toxicities include mucositis, severe pain, and difficulty swallowing, while late toxicities include xerostomia, trismus, hearing impairment, temporal lobe necrosis, cognitive impairment, cranial nerve injuries, osteoradionecrosis, and carotid artery involvement. Radyonecrosis is one of the most difficult complications to treat after radiotherapy for nasopharyngeal carcinoma. We aimed to evaluate our case who developed deep neck infection with osteoradionecrosis after receiving chemoradiotherapy following nasopharyngeal cancer, in the light of the literature.IntroductionNasopharyngeal carcinoma is an epithelial neoplasm that originates from the mucosa of the nasopharynx, it is most commonly observed in Rosenmüller fossa. The incidence is high in Southeast Asia, particularly in Southern China (80-120 / 100,000), while it is rare in North America and European countries (0.5-1 / 600,000). The most commonly affected age ranges are adolescence and the 4th-5th decades, with a prevalence 4-5 times higher in men than in women [1]. Clinical manifestations include unilateral effusion in otitis media, presence of neck masses, pain in the temporal and facial regions, and in advanced stages, bloody nasal discharge and nasal obstruction can be seen [2]. The primary treatment is radiotherapy(RT) [3]. Acute toxicities include mucositis, severe pain, and difficulty swallowing, while late toxicities include xerostomia, trismus, hearing impairment, cranial nerve injuries, osteoradionecrosis, and carotid artery involvement [4]. The incidence of radiation-induced osteoradionecrosis in nasopharyngeal carcinoma is 0.8-1.1%, making it one of the most difficult-to-treat complications [5]. The pathophysiology is uncertain, however hypoxia, hypovascularity, and hyposellularity are thought to play a role in its development [6]. We aimed to evaluate our case who developed deep neck infection with osteoradionecrosis after receiving chemoradiotherapy following nasopharyngeal cancer, in the light of the literature. Case ReportThe 67-year-old male patient presented to our clinic with complaints of a neck mass, nasal congestion, and hearing loss. The patient has no significant medical history but has been smoking a pack of cigarettes a day for 10 years. In the physical examination, a 2x1 cm hard and fixed mass was found on the left level II of the neck, and the left tympanic membrane had a dull appearance and was retracted. Endoscopic examination revealed a mass involving the posteriosuperior of the nasopharynx, the posterior and floor of the septum, and the posterior of both conchae, which was advancing at the base of both nasal passages and contained necrotic tissues. MRI(Magnetic resonance ımaging) of the nasopharynx and neck showed a solid mass lesion of approximately 43x29x34 mm in size with irregular borders, progressing towards both nasal passages filling the nasopharynx, showing enhancement (Figure 1).
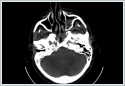
There were lymphadenopathies of approximately 2 cm in diameter in the bilateral submandibular region and cervical chain. Bilateral paracentesis was performed under general anesthesia, ventilation tubes were placed in both ears, and a biopsy was taken from the nasopharynx. The pathology result revealed non-keratinized nasopharyngeal carcinoma of undifferentiated subtype. Treatment and Prognosis The patient was presented to the tumor board and discussed. According to the TNM staging system of the American Cancer Joint Committee (8th edition, 2017), the patient was classified as T3N2M0. Chemoradiotherapy was decided upon following induction chemotherapy. The patient received three cycles of Cisplatin+Gemcitabine. Subsequently, the patient was treated with LINAC device to the nasopharynx and bilateral longitudinal 6MV X-ray with 200cGy/day fraction five days a week for 6000 cGy, boost to the primary lesion 6MV X. 7000 RT was applied with irradiation. Cisplatin 75mg/m2/day was administered concomitantly with RT on the 1st, 22nd and 43rd days. The patient experienced only mucositis as a side effect in the early period after RT. The patient presented to our clinic 6 months later with severe headache, nausea, and severe pain with neck movements. The headache was compressive, starting from the mastoid and spreading to the entire head, but it was not affected by light, sound, or change in position. Although the patient's neck pain increased with flexion, but Kernig and Brudjenski tests were negative. The patient also reported suicidal thoughts due to the severity of the pain. During physical examination, he was conscious, oriented, cooperative, pupils were isochoric, eyes were mobile in all directions, and other neurological examinations were normal. The right tympanic membrane was dull, and extensive necrotic tissue was observed in the nasopharynx during endoscopic examination. Destruction and cortical irregularities were observed in the lower wall of the sphenoid sinus and anterior wall of the clivus in computerized tomography(CT) (Figure 2).
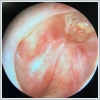
The patient was consulted to the neurology to rule out central pathologies, and central pathologies were excluded. Because of her severe pain, he was consulted to the infectious diseases department in terms of algology and excluding central nervous system infection and for advise antibiotic therapy. The patient was diagnosed with a deep neck infection and started on analgesics and antibiotics, receiving parenteral antibiotic therapy for 28 days. A biopsy was taken from the necrotic tissue containing the mucosa (Figure 3) in the superior midline of the nasopharynx under general anesthesia. The pathology report showed necrotic tissues.
After the treatment, the patient's pain decreased and the infection was reduced based on the follow- up tomography. However, the necrotic tissue did not show any improvement. The patient was discharged after being referred to hyperbaric oxygen therapy. The patient received a total of 30 sessions of hyperbaric oxygen therapy at 2.4 ATA pressure in the multi-person pressure chamber. The patient experienced a significant decrease in pain and improved head and neck movements.
Control CT and endoscopic examinations(Figures 4,5) showed a significant regression in the signs of infection and the necrotic area. The patient's clinical comfort was ensured and a return to social life was achieved. Clinical follow-up of the patient continues DiscussionRadyonecrosis is one of the most difficult complications to treat after RT for nasopharyngeal carcinoma [8]. Necrosis can spread from the mucosa to the para-pharyngeal tissues or skull base, leading to severe headaches, bad odors, cervical instability due to osteoradionecrosis, and dysphagia due to 10th cranial nerve involvement in patients. Radyonecrosis are classified in the literature into three stages: early, middle, and late. Early-stage patients show only mucosal necrosis, while middle-stage patients show necrosis of mucosa, muscle, and tendon. Late-stage necrosis includes osteoradionecrosis [7]. In our case; mucosal, muscle, and tendon necrosis were seen on endoscopic examination, and irregularities were observed on Clivus, so it was classified as late-stage radyonecrosis. The most commonly used treatment for radyonecrosis is conservative treatment with repeated endoscopic debridement. However, this treatment is limited due to difficulties in completely removing necrotic tissue and injury of the skull base bone, dura, or carotid artery. Injury to the internal carotid artery is the worst prognostic factor for nasopharyngeal radyonecrosis [5]. The benefits of hyperbaric oxygen theraphy (HOT) on radiation-induced bone and soft tissue necrosis are known in the maxillofacial region, mouth, and head and neck lesions. HBO increases tissue pO2 and initiates a cellular and vascular repair mechanism. Leber et al. have shown in their study that HBO is an effective method for treating radiation-induced side effects [9]. Informed ConsentInformed consent form was obtained from the case himself.References
|
|||||||||||
| Keywords : nazofarinks , nazofarinks karsinomu , kemoradyoterapi , radyoterapi , osteoradyonekroz , derin boyun enfeksiyonu | |||||||||||
|