|
|||||||
AbstractTuberculosis of the head and neck region typically presents with more involvement of lymph nodes. It should be noted, especially in older patients, that it can be mistaken for malignancy. Tuberculosis involvement in the hypopharynx is particularly rare. It should be considered in the differential diagnosis in young patients. After confirmation of diagnosis through biopsy or culture, treatment for patients should be determined through a multidisciplinary approach.IntroductionEach year, tuberculosis (TB) imposes a significant burden, with over eight million new cases reported and 1.3 million lives lost [1]. Primarily concentrated in Southeast Asia (44%), Africa (24%), and the Western Pacific (18%), TB's impact is widespread across nearly all global regions [2]. Extrapulmonary presentations account for 20% of all TB cases [3], with head and neck involvement affecting 10% of affected individuals [4]. Notably, TB affecting the head and neck primarily manifests in lymph nodes, but involvement in the larynx, middle ear, oropharyngeal mucosa, salivary glands, paranasal sinuses, or the prevertebral space has also been documented [5,6] Herein, we present a clinical case of tuberculosis with an unusual localization: the pyriform sinus. Case ReportA 33-year-old female patient presents to the outpatient clinic with a complaint of sensation of throat obstruction and dysphagia persisting for the past 4 months. There is no history of weight loss or night sweats. The patient denies any history of tobacco or alcohol use. There are no remarkable features in the clinical history. Additionally, no significant data are identified in the patient's family history. Informed contest was taken from the patient. During the patient's endoscopic examination, edema was observed in the right arytenoid and aryepiglottic fold. Additionally, there was medial fullness in the right piriform sinus (Figure 1).
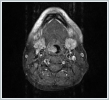
There is no findings of physical examination such as nodal involvement. Contrast-enhanced neck magnetic resonance imaging (MRI) revealed a mass measuring 25*12 mm at the level of the aryepiglottic fold, demonstrating hypointensity on T1-weighted images, hyperintensity on T2-weighted Images, and intense contrast enhancement in the right piriform sinus region (Figure 2). Following imaging, multipl biopsies wer performed with direct laryngoscopy under general anesthesia.
The pathology results revealed necrotizing granulomatous inflammation and the presence of multinucleated benign giant cells (Figure 3). Further investigations conducted for tuberculosis (TB) in the patient yielded results supportive of extrapulmonary tuberculosis. Subsequently, the patient was initiated on tuberculosis treatment.
DiscussionBetween 2002 and 2011, extrapulmonary involvement was identified in 19.3% of the 868,726 reported cases of tuberculosis [3]. Lymphatic involvement predominates in the head and neck region. Hypopharyngeal tuberculosis has been scarcely documented in the literature [7-9]. The microorganism Mycobacterium tuberculosis primarily induces extrapulmonary involvement via lymphatic and hematogenous dissemination. Its resemblance to hypopharyngeal cancer is notably significant, necessitating careful consideration. Suspicious indicators in the patient's medical history encompass youthfulness and the absence of smoking and alcohol consumption habits. Endoscopic biopsy is imperative for establishing the diagnosis of hypopharyngeal tuberculosis. It serves a dual purpose of confirming the diagnosis and ruling out potential malignancy. While tuberculosis culture remains the gold standard for diagnosis, its implementation may extend the diagnostic timeline. Thus, the presence of necrotizing granulomatous inflammation and acid-fast bacilli (AFB) stained by Ziehl-Neelsen in pathology are frequently relied upon during the diagnostic evaluation. According to the literature, many cases of tuberculosis in the head and neck region present with lymph node involvement [10]. In the study by Gehrke et al., it was observed that while tuberculosis diagnosis is generally easier to establish in patients under the age of 40 (68.75%), in patients over the age of 40, malignancy was initially diagnosed (57.89%), leading to delayed tuberculosis diagnosis [11]. Histopathological examination, polymerase chain reaction (PCR), microbiological culture, and interferon-gamma-release-assay (IGRA) are used for diagnosis. Histopathologically, 80% of patients exhibit necrotizing granulomatous inflammation [11]. Primary hypopharyngeal tuberculosis represents an exceptionally uncommon phenomenon. The pivotal consideration lies in excluding the potential for malignancy. Particularly in regions where tuberculosis prevails and instances of tuberculosis manifesting at a young age, meticulous assessment of the differential diagnosis assumes paramount importance. AcknowledgementFunding: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declarations of interest: none Informed ConsentThe informed consent was taken from the patientsReferences
|
|||||||
| Keywords : Tüberküloz , Hipofarinks , Baş ve Boyun | |||||||
|