|
|||||||||
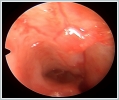
AbstractDermoid cyst is a type of benign hamartoma that often occurs on the skin of the head and neck in infants or children, but can sometimes also occur in adults without an apparent familial transmission. It is a rare condition that occurs once in 20,000 to 40,000 births. Dermoid cyst usually appears as a painless, slow-growing lesion and is diagnosed at the age of 1-3 years. About 3% of dermoid cysts are located in the nasal midline, including the glabella, nasal dorsum, and columella. Due to the connection between the nasal and cranial cavities, the presence of deep appendages and communication of the central nervous system is possible. In this article, we presented our experience with the surgical removal of the cyst tract in the nasal dorsum of a 4-year-old female patient who was operated for intracranial dermoid cyst 5 months ago, accompanied by the literature.IntroductionNasal dermoid cysts are rare congenital lesions of ectodermal and mesodermal origin [1]. A rare occurrence in children with presentation in one out of 20 000–40 000 births [2]. Dermoid cyst usually presents as a painless, slow-growing lesion that is diagnosed within the age of 1-3 years [3]. Most of the lesions present as dermal sinuses or cysts in the midline of the nasal dorsum [4]. A tract can exist from the nasal dorsum to the anterior cranial fossa [5]. The differential diagnoses of midline nasal masses include gliomas, encephaloceles, epidermoid cysts, and hemangiomas [6]. The most widely accepted cranial theory states that in the early embryo, the dura is in contact with the skin and separates as the frontal bone forms between them. The failure of separation during this process leads to dermoid cyst formation [7]. During the surgical removal of dermoid cyst, intracranial communication is possible; therefore, an exclusion is required before biopsy or surgical intervention [3]. The use of magnetic resonance imaging (MRI) helps not only in the diagnosis of dermoid cyst but also in ruling out the presence of any intracranial communication [8]. The accepted treatment is complete surgical excision. Meticulous surgical planning is a must to avoid unexpected surgical situations. The nasal location of the lesions and probable involvement of deeper structures together with the possibility of an intracranial extension necessitate full clinical and radiological assessments before excision to prevent complications and local recurrence [5]. Case ReportA 4-year-old female patient applied to us with complaints of redness, swelling, and a purulent wound at the tip of the nose. On physical examination, a reddened lesion with a size of approximately 2x2 mm, raised from the skin, was observed in the nasal supratip region. (Picture 1) The patient who was operated on at an external center with the diagnosis of left frontal intracranial dermoid cyst about 5 months ago was hospitalized and antibiotherapy treatment was given. Contrast-enhanced brain MRI " A soft tissue lesion of approximately 6 mm in diameter, slightly hyperintense, was noted in the midline T1-T2 sequences in the cutaneous-subcutaneous soft tissue planes of the nasal dorsum. It may be a dermoid or sebaceous cyst.”
The patient underwent dermoid cyst excision and open rhinoplasty incision under general anesthesia. Nasal tip skin and nasal dorsum were elevated with a midcolumellar W incision. The tunnel formed by the fistula tract of the dermoid cyst starting from the caudal tip of the nose as intercolumellar in the upper middle part of the septum was followed up to the skull base and excised. (Picture 2) The tunnel was filled with soft tissue and tissue adhesive to avoid potential voids. The surgical specimen sent to pathology was reported as "Findings compatible with a ruptured dermoid cyst". (Picture 3) The postoperative 6th-week image of the patient is attached. (Picture 4)
DiscussionDermoid cyst is a kind of benign hamartoma, which often occurs in the skin of head and neck in infants or child, but sometimes may occur in adults with no obvious familial inheritance [9]. Nasal dermoid cysts account for 13% of all dermoids and 4 to 12% of head and neck dermoids [10]. The most common location is in the orbital ridge region, with no association or deep extension [8]. Approximately 3% of dermoid cysts are located in the nasal midline, including the glabella, nasal dorsum, and columella. Because of the connection between the nasal and cranial cavities, the presence of deep extension and central nervous system communication is possible. Therefore, MRI should be performed for midline masses before further invasive procedures to prevent complications, such as meningitis [11]. Dermoid cyst pathology showed that the cyst was unilocular, with thick wall, similar to complete, or incomplete skin structure. The innermost layer is cuticle, and the other layers are granular layer, spinous cell layer, basal layer, and dermis. In the dermis, there are hair follicles, sebaceous glands, eccrine glands, and apocrine sweat glands. Keratinizing, stratified squamous epithelial lining, intraluminal keratin, sebum, epithelial debris, hair, and viscous fluid could be seen in the capsule [12]. Complete resection of the entire cyst wall is the best treatment. If the cyst is closely connected with important structures, the cyst wall may not be completely removed by surgery, which may lead to recurrence. If the dermoid cyst is repeatedly infected, it may lead to intracranial infection, abscess, and even death [13]. The external rhinoplasty approach, especially in young children with thin stretched skin over a distended cyst, is surgically demanding. Other approaches include a vertical midline skin incision over the cyst, transnasal endoscopic removal, transverse nasal incision, medial canthal incision, eyebrow incision, gull-wing incision and bi-coronal flap, all of which have been advocated along with external rhinoplasty for nasal dermoids [1,5]. In a recent large case series, they reported that lesions with intracranial extension constitute approximately 10% of all nasal dermoid cyst. Furthermore, they proposed that classification may be performed on the basis of lesion depth or extent, which allowed proper surgical planning [4]. The authors suggested that intracranial–extradural lesions could be excised through limited frontonasal osteotomy, while bicoronal flap with frontal craniotomy is suitable for intracranial– intradural lesions . Other studies advocated traditional craniotomy for the total removal of intracranial dermoid,[14] but some studies have noted the success of endoscopic endonasal approach for intracranial extension of nasal dermoid cyst [15]. ConclusionAs a result, dermoid cyst can be considered as a pre-diagnosis in painless and slow-growing lesions that often occur in the midline of the head and neck skin in children and infants. Early diagnosis and treatment are important as there is a possibility of intracranial spread. References
|
|||||||||
| Keywords : Pediatrik , dermoid kist , intrakranial | |||||||||
|