Abstract
Solitary fibrous tumors (SFTs) are fibroblastic mesenchymal tumors , first defined in the pleura and rarely observed in the floor of the mouth.They usually present as a painless swelling.Radiographic findings of SFT are similar to those of other soft tissue tumors.The definitive diagnosis is based on the examination of morphological and immunohistochemical findings after excision of the lesion.In this article, a case of solitary fibrous tumor in the floor of the mouth in a 28-year-old male patient is discussed in the light of the literature.
Introduction
Solitary fibrous tumors (SFT) include tumors previously classified as hemangiopericytoma, rarely metastasizing, and generally affecting the pleura [1]. Histologically, they consist of fibroblastic mesenchymal cells. Consistent with the mesenchymal origin of SFT, this tumor has been documented in nearly every anatomical location, with both benign and malignant variants described [2].
Extracranial SFT in the head and neck region constitute about 10% of cases [3], typically small and symptomatic tumors, most commonly seen along the sinonasal tract and orbit [4]. These types of tumors are rare in the oral cavity but, when examined in the literature, are most frequently found in the buccal mucosa and cheek [5].
When SFT develops in the oral cavity, it presents as a painless swelling, and some may cause compression symptoms as they reach larger sizes. The differential diagnosis includes lipomas, pleomorphic adenomas, schwannomas, fibrous histiocytomas, benign glandular tumors, and dermoid cysts.
On sectional imaging (computed tomography [CT] and magnetic resonance imaging [MRI]), the radiographic findings of SFT are similar to those of other soft tissue tumors, with no specific pathognomonic features [6].
The diagnosis of SFT requires a histological examination of an adequate tissue sample, recognizing typical morphological features combined with a characteristic immunophenotype. Complete resection of the tumor is required for full histopathological evaluation. Fine needle aspiration biopsies are usually inadequate and not recommended for diagnosis.
Case Report
A 28-year-old male patient presented to our outpatient clinic with a complaint of painless swelling inside the mouth for about two months. On examination, there was a firm, mobile, solid mass lesion approximately 3 cm in size with deep extension, covered by intact mucosa on the left floor of the mouth. No additional pathological findings were noted on further examination.
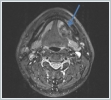
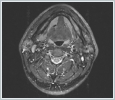
Contrast-enhanced neck MRI revealed a signal area approximately 40x20x30 mm in size, heterogeneously hypointense in the T1A , sequence and hyperintense in the T2A sequence at the level of the oropharynx on the left floor of the mouth, showing no pathological contrast enhancement after intravenous contrast administration and having relatively smooth contours [Figure 1].
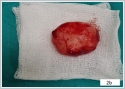
The patient operated under general anesthesia. A 2 cm mucosal incision was made lateral to the Wharton duct on the left floor of the mouth. The lesion was separated from the underlying muscle layer and lateral mandible with the help of a clamp [Figure 2a]. The excisional biopsy material was a solid, cream-white, firm nodule measuring 35x35x17 mm in a single piece [Figure 2b].
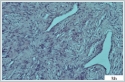
Histopathological examination showed a mesenchymal lesion with encapsulated well-defined boundaries, without evidence of capsule invasion. No mitotic activity, significant cytological atypia, or necrosis was observed [Figure 3].
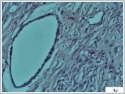
Immunohistochemical examination revealed pansitokeratin-negative, CD34-positive, CD99-positive, desmin-negative, smooth muscle actin-negative, CD68-negative, and S100-negative staining [Figure 4].
The morphological and immunohistochemical findings were consistent with a diagnosis of solitary fibrous tumor/hemangiopericytoma.
Postoperative contrast-enhanced neck MRI showed that the lesion had been totally resected, with no signs of recurrence [Figure 5].
The patient was followed up with regular clinical evaluations for about one year, with no evidence of recurrence.
Discussion
SFT was first described by Klemperer et al. in 1931 in the lungs and pleura [7]. It is classified by the World Health Organization (WHO) as a borderline/low-grade fibroblastic tumor that rarely metastasizes [8]. Based on patient age, tumor size, mitosis, and necrosis criteria, these tumors are classified as high-risk, medium-risk, or low-risk for metastasis [9].
Oral cavity SFT is typically described as a solitary submucosal, well-defined, firm, rubbery, asymptomatic nodule of varying sizes. On examination, it usually appears as a smooth, firm, white nodular mass [10].
In CT imaging, SFT appears isodense or hypodense compared to adjacent muscle systems or as a combination of both [11]. In MRI, SFT typically shows low signal intensity on T1-weighted images and low or mixed-high signal intensity on T2-weighted images [11].
However, imaging features of SFT on the floor of the mouth are not specific. Therefore, other lesions in this region should also be considered, including minor salivary gland tumors such as pleomorphic adenomas, lipomas, schwannomas, fibrous histiocytomas, benign glandular tumors, and dermoid cysts.
Due to the wide morphological variability of SFT, diagnosis can be challenging [12]. Definitive diagnosis is made by immunohistochemistry, distinguishing it from other mesenchymal tumors [19]. SFT have a characteristic immunohistochemical profile [13].
According to the study by Nunes et al., 99% of benign cases were positive for CD34, 93% for BCL2, and 71.4% for CD99 immunohistochemically. Smooth muscle actin, S100, desmin, and cytokeratin were generally negative [10]. In our case, CD34 was positive, CD99 was positive, desmin was negative, smooth muscle actin was negative, and S100 was negative [Image 4]. Recently, the NAB2/STAT6 fusion gene has been found to be a common finding in almost all SFT [14], and since then, it has been widely adopted as a reliable diagnostic marker [9]. However, in our case, the NAB2/STAT6 fusion gene could not be evaluated.
Most SFTs are well-defined and partly encapsulated within the submucosa, making excision easier [15]. In our case, the lesion was well-defined during surgery, with a capsule present on microscopic examination, and there was no capsule invasion [Image 3d].
Complete surgical excision is curative in most cases of SFT. Predicting behavior based on histological criteria alone is not possible. Even in the presence or absence of atypical histological features, SFT may recur or metastasize after total resection [12]. Long-term follow-up is recommended for all SFT due to the possibility that these lesions are not entirely benign [16,19].
In cases where surgical excision is not possible, the use of adjuvant therapies such as radiotherapy and chemotherapy has been reported [17,18].
Conclusion
In rare cases, SFT should be included in the differential diagnosis of lesions in the oral cavity. There is no specific finding of SFT by imaging methods. Clinical, pathological and immunohistochemical features are of great importance in diagnosing the tumor. Although it rarely metastasizes, follow-up is important for a prognosis.
Informed Consent
kendinden
References
- Tavora F, Calabrese F, Demicco EG. Toraksın soliter fibröz tümörü. In: Torasik Tümörler, 5. baskı, WHO Tümör Sınıflandırması Editör Kurulu (Ed), IARC Press, 2021.
- Demicco EG, Fritchie KJ, Han A. Solitary Lifli Tümör. Yumuşak Doku ve Kemik Tümörleri, 5. baskı, WHO Tümör Sınıflandırması Editör Kurulu (Ed), IARC Press, 2020. s.104.
- Smith SC, Gooding WE, Elkins M, ve diğerleri. Baş ve Boyunun Soliter Lifli Tümörleri: Çok Kurumsal Klinikopatolojik Bir Çalışma. Am J Surg Pathol 2017; 41:1642.
- Bernardini FP, de Conciliis C, Schneider S, ve diğerleri. Orbitanın soliter fibröz tümörü: nadir midir? Bir vaka serisinin sunumu ve literatürün gözden geçirilmesi. Oftalmoloji 2003; 110:1442.
- Satomi T, Hasegawa O, Abukawa H, Kohno M, Enomoto A, Chikazu D. Yanakta ortaya çıkan olağanüstü büyük tekil fibröz tümör: Literatür taramasıyla birlikte immünohistokimyasal ve ultrastrüktürel bir çalışma. Med Mol Morphol. 2014;47:108–11.
- Chick JF, Chauhan NR, Madan R. Toraksın soliter fibröz tümörleri: isimlendirme, epidemiyoloji, radyolojik ve patolojik bulgular, ayırıcı tanı ve tedavi. AJR Am J Roentgenol 2013; 200:W238.
- Klemperer P, Rabin CB. Plevranın primer neoplazmı: Beş vaka raporu. Arch Pathol. 1931;11:385–412.
- Tariq MU, Din NU, Abdul-Ghafar J, Park YK. Soliter fibröz tümörün birçok yüzü; histolojik özelliklerin çeşitliliği, ayırıcı tanı ve yanlış tanıyı önlemede ve davranışı tahmin etmede moleküler çalışmaların ve vekil belirteçlerin rolü. Diagn Pathol. 2021;16(1):32.
- Anderson WJ, Doyle LA. 2020 Dünya Sağlık Örgütü yumuşak doku ve kemik tümörleri sınıflandırmasından güncellemeler. Histopatoloji. 2021;78(5):644–657.
- Nunes FB, Sant'Ana MSP, Silva AMB, Agostini M, Silva Canedo NH, de Andrade BAB, ve diğerleri. Ağız boşluğunun soliter fibröz tümörü: bir güncelleme. J Oral Pathol Med. 2020;49(1):14–20.
- Papathanassiou ZG, Alberghini M, Picci P, Staals E, Gambarotti M, Garaci FG, ve diğerleri. Yumuşak dokuların soliter fibröz tümörleri: histopatolojik korelasyonlarla görüntüleme özellikleri. Clin Sarcoma Res. 2013;3(1):1.
- Sánchez-Legazaa E, Guerrero-Cauquib R, Caravallo JIM, Murga Tejada C. Pürüzsüz Damakta Soliter Fibröz Tümör. Acta Otorrinolaringol Esp. 2011;62:239–41.
- Gonzalez-Garcia R, Gil-Diez Usandizaga JL, Hyun Nam S, Rodriguez Campo FJ, Naval-Gias L. Agresiflik histolojik özelliklerine sahip oral boşluğun soliter fibröz tümörü. Br J Oral Maxillofac Surg. 2006;44:543–5.
- Mohajeri A, Tayebwa J, Collin A, Nilsson J, Magnusson L, von Steyern FV, ve diğerleri. Kapsamlı genetik analiz, patognomonik bir NAB2/STAT6 füzyon genini, rastgele olmayan ikincil genomik dengesizlikleri ve tekil fibröz tümörde karakteristik bir gen ekspresyon profilini tanımlar. Genler Kromozomlar Kanser. 2013;52(10):873–886.
- Li XM, Yu JQ, Xu GH. Yumuşak damağın soliter fibröz tümörü: İki vaka raporu. Onkoloji Mektupları. 2014;7:1975–1977.
- Ogawa I, Sato S, Kudo Y, Miyauchi M, Sugiyama M, Suei Y. Dil altı bezinde ortaya çıkan kötü huylu potansiyele sahip soliter fibröz tümör. Pathol Int. 2003;53:40–5.
- Yang XJ, Zheng JW, Ye WM ve diğerleri. Baş ve boynun kötü huylu tekil fibröz tümörleri: dokuz ardışık hastada yapılan klinikopatolojik bir çalışma. Oral Onkoloji. 2009;45(8):678–682. doi: 10.1016/j.oraloncology.2008.10.013.
- Cox DP, Daniels T., Jordan RCK Baş ve boynun soliter fibröz tümörü. Ağız Cerrahisi, Ağız Tıbbı, Ağız Patolojisi, Ağız Radyolojisi ve Endodontoloji. 2010;110(1):79–84. doi: 10.1016/j.tripleo.2010.01.023.
- De Morais EF, Martins HDD, Rodrigues KS, de França GM, da Silveira ÉJD, Freitas RA. Clinicopathologic Analysis of Oral and Maxillofacial Solitary Fibrous Tumor. Am J Clin Pathol. 2020 Jun 8;154(1):15-22. doi: 10.1093/ajcp/aqaa027. Erratum in: Am J Clin Pathol. 2024 Jun 26. doi: 10.1093/ajcp/aqae086. PMID: 32134474.
Presented at
15 – 19 Kasım 2023 tarihleri arasında Kaya Palazzo Kongre Merkezi'nde katılım sağlandı 44. Türk Ulusal KBB BBC Kongresi'nde elektronik poster olarak sunuldu.
|