|
|||||||||
AbstractLeishmaniasis are a group of parasitic diseases caused by leishmania species and transmitted through the bite of an infected female sandfly. Leishmaniases present a wide spectrum of clinical manifestations including cutaneous (CL), diffuse cutaneous (DCL), mucocutaneous (MCL), and visceral leishmaniasis (VL)[1]. Its incidence is on the rise in certain geographic areas of the world, including Syria, Turkey, and Jordan, due to war-associated migration and the resulting refugee crisis. CL can be confused with other diseases such as neoplasia ,and mycotic infection, , pyoderma gangrenosum, lupus vulgaris, lupus erythematosus, sarcoidosis, and granuloma annulare[2].Based on the history and physical examination of the patient who applied with the complaint of persistent ulcer on the lower lip, we considered squamous cell cancer as a preliminary diagnosis and performed a biopsy. The biopsy result was reported to be compatible with plasmacytoma. The patient's history and the results of the examinations did not support the plasmacytoma, so we performed a biopsy again, and the biopsy was compatible with leishmania. We will discuss leishmania and diseases that are confused with leishmania by reviewing the current literatureIntroductionLeishmaniasis are a group of parasitic diseases caused by leishmania species and transmitted through the bite of an infected female sandfly. Leishmaniases present a wide spectrum of clinical manifestations including cutaneous (CL), diffuse cutaneous (DCL), mucocutaneous (MCL), and visceral leishmaniasis (VL) [1]. Its incidence is on the rise in certain geographic areas of the world, including Syria, Turkey, and Jordan, due to war-associated migration and the resulting refugee crisis. CL can be confused with other diseases such as neoplasia ,and mycotic infection, , pyoderma gangrenosum, lupus vulgaris, lupus erythematosus, sarcoidosis, and granuloma annulare [2].Based on the history and physical examination of the patient who applied with the complaint of persistent ulcer on the lower lip, we considered squamous cell cancer as a preliminary diagnosis and performed a biopsy. The biopsy result was reported to be compatible with plasmacytoma. The patient's history and the results of the examinations did not support the plasmacytoma, so we performed a biopsy again, and the biopsy was compatible with leishmania. We will discuss leishmania and diseases that are confused with leishmania by reviewing the current literature. Case ReportA 73-years old male came to the otorhinolaryngology out-patient department with a complaint of a a lesion on his lower lip for the last 3 years. Lesion started as a small red papule which gradually increased in size with central crusting.The patient lives by farming in the village. The patient has been smoking a pack of cigarettes a day for 50 years.There was no other significant family or medical history. There was no history of going out of the village until our examination. Clinical examination showed an indurated, crusted ulcer with swelling on the midline of the lower lip (Figure 1).
General physical examination did not show anything pathological; in particular, regional lymph nodes were not involved. Since the patient had persistent ulcers, smoking history, and a history of sun exposure, squamous cell cancer was considered as a preliminary diagnosis and contrast enhaced magnetic resonance imaging (MRI) was performed. MRI showed that a lesion of approximately 28*12 mm in the axial plane of the lower lip was detected with intermediate signal on T1W and T2W examinations, mild contrast enhancement on postconstast images, and mild diffusion restriction on diffusion-weighted examination (Figure 2,3).
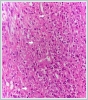
Then, an incisional biopsy was performed from the mass to include intact tissue. Biopsy material was reported as ulcer floor rich in plasma cells. According to the biopsy result, the patient was consulted to the hematology department with a preliminary diagnosis of plasmacytoma. Plasmocytoma was not considered by the hematology department because complete blood count smear, blood sedimentation rate, kidney function, electrolyte (calcium), serum and urine protein electrophoresis, quantitative Ig determination in serum, immunoelectrophoresis determination of serum and urine and B-2 microglobulin was within normal limits. Incisional biopsy was performed again from the patient's lesion. Biopsy material was reported as donovan bodies compatible with leishmania(Figure 4).
As the biopsy result was compatible with leishmania, the patient was referred to the dermatology department. Intralesional glucantime treatment was started once a week by the dermatology department. The patient's lesion completely regressed after receiving intralesional glucantime therapy 12 times. DiscussionSquamous cell carcinoma (SCC) of the lower lip is a common malignant tumor that accounts for 25% to 30% of all oral cancer [3]. It occurs most frequently in male patients ,aged 50 years[3]. Those working outdoors and in the countryside are at higher risk, as chronic sun exposure is the strongest risk factor [3]. Lip SCC most frequently begins as ulcerative lesions known as actinic cheilosis. Any nonhealing ulcerative lesion of the lip or oral cavity warrants a biopsy for histopathologic analysis. Diagnosis of SCC is ultimately achieved with tissue biopsy [4]. Plasma cell is seen in microscopic examination of many diseases, for example oral plasma cell mucositis,erosive lichen planus, mucous membrane pemphigoid, sarcoidosis, extramedullary plasmacytoma, squamous cell carcinoma, and some infectious diseases(leishmania, syphilis, Castleman’s disease, fungal infections a primary infectious disease of the lymph node, and, in recent times, COVID-19. Plasma cell mucositis is an idiopathic disease characterized histologically by dense lymphocyte and plasma cell infiltrates in the submucosa, with lesions usually seen on the mucosal surfaces, vulva and penis, gums, lips, tongue, buccal mucosa, epiglottis and larynx. Lichen planus is a chronic-relapsing inflammatory disease, with cutaneous and mucous involvement. Lichen planus is identified with bilateral and symmetrical lesions that is white patches with erosive aspects moreover, a hyperkeratosis is observed in the lower epidermis and in the upper dermis histologically.Mucous membrane pemphigoid is a heterogeneous group of chronic, autoimmune subepithelial blistering diseases which predominantly involves the mucous membranes and occasionally the skin. In vivo, it is characterized by linear deposition of IgG, IgA, or C3 along the epithelial basement membrane zone. Sarcoidosis is a rare acquired systemic granulomatous disease. Oral lesions of sarcoidosis can be solitary or multiple; they appear as a well-delimited and occasionally ulcerated red swelling [6]. Plasmacytoma, a plasma cell disorder, is an extramedullary variant of multiple myeloma. There are two types of plasmacytomas — solitary plasmacytoma of bone (SPB) and extramedullary plasmacytoma (EMP). The majority of extramedullary plasmacytomas are found in the head and neck region. Primary cutaneous plasmacytomas present as relatively slowly growing papules or plaques, or as a solitary tumor or a multisite erythematous purplish nodule. Symptoms vary depending on the location and size of the lesion. Weakness, night sweats and weight loss are rarely seen in patients with plasmacytoma. Histologically, it shows dermal infiltrate of plasma cells at different maturation stages. The median age at diagnosis is 60 years, predominantly male and usually seen in Asian people [5]. Plasma cell infiltrate is seen in Candida Albicans infection because it is a delayed hypersensitivity reaction.The histopathological features of syphilis are inflammatory infiltrates containing plasma cells, lymphocytes, and macrophages, usually with a perivascular distribution [6]. Leishmaniasis is a parasitic infection caused by species of the genus leishmania. The disease is transmitted by the bite of female sandflies belonging to the Phlebotomus family. It can also be transmitted by congenital, transfusion, organ transplant, laboratory accidents[1]. In the midge, the parasites are present in the promastigote form. Macrophages in the dermis phagocytize promastigotes, which are then transformed into intracellular non-flagellate amastigotes known as leishman Donovan bodies [7]. Cutaneous, mucocutaneous and visceral leishmaniasis are three main clinical forms of the disease. Cutaneous leishmaniasis (CL) is most common form of leishmaniasis.Cutaneous leishmaniasis is not life-threatening, but can lead to serious cosmetic morbidity, social stigma, and psychological effects [7]. CL usually begins as a small papule at the site of inoculation on an exposed body area such as the head or extremities. This papule gradually becomes a nodule and then ulcerates. In general, patients are systemically well although the lesions are sometimes itchy, they do not produce the pain one might expect from their appearance. The characteristic ulcer of CL heals on its own within 3 to 18 months, depending on the particular type. It is estimated that up to 10% of CL cases progress, become chronic and exhibit more severe clinical features(3).The diagnosis is confirmed by identification of the parasite in a smear, biopsy or tissue culture [1]. Histopathological examination is an important diagnostic tool that can help differentiate between conditions mimicking CL. A biopsy should be taken to include the affected and unaffected part of the ulcer or nodüle [8]. Generally, there is no single 100% effective treatment for leishmaniasis. Antimonial compounds are still considered first-line therapy for cutaneous leishmaniasis[1]. Lip involvement can be treated with intralesional injections, systemic therapy, or combinations of these depending on the clinical picture and the infective species.Intralesional injections can cause burning sensation, pain, inflammation and vasovagal reaction. For CL, 12 months of follow-up is recommended [9]. References
|
|||||||||
| Keywords : Leishmania , Kutanöz Leishmania , Skuamöz Hücre Karsinoması , Plazma Hücresi | |||||||||
|