|
|||||
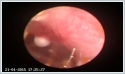
AbstractWe present a rare case of tympanic membrane cholesteatoma (TMC) in a 2 year-old girl. Pediatric congenital cholesteatomas are rare and generally asymptomatic, making it difficult for otorhinolarygologists and pediatricians to diagnose early. Congenital cholesteatomas within the tympanic membrane (TM) are even more rare. Early diagnosis and treatment of TMC is essential to avoid progressive destruction in the ear. A whitish spot on the TM should raise suspicion for cholesteatoma. In differential diagnosis, tympanosclerosis, foreign bodies, keratosis obliterans and cholesterol granuloma always should be kept in mind.IntroductionPediatric congenital cholesteatomas are rare and generally asymptomatic, making it difficult for otorhinolarygologists and pediatricians to diagnose early. Congenital cholesteatomas within the tympanic membrane (TM) are even more rare. Tympanic membrane cholesteatoma (TMC) was first described in 1863 by Hinton [1,2]. Less than 25 cases of TMC without previous otorrhea or ear surgery have been reported to date in the literature [3-8]. Early diagnosis and treatment is essential since the lesion can advance just like any other cholesteatoma. A white spot on TM should raise suspicion for TMC [9]. We present a 2 year-old girl with left TMC located in the posterosuperior quadrant. Case ReportA 2 year-old girl was presented to our outpatient clinic with persistent coughing for 2 months. Otolaryngologic examination did not reveal any abnormality except left TM. Otomicroscopic examination revealed a 2 mm whitish, clearly shaped, non-pulsatile mass at the posterosuperior quadrant of TM (Figure 1).
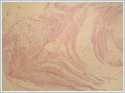
Patient had no history of ear infection, otorrhea, trauma or ear surgery. Tympanograms were A type bilaterally. Acoustic reflexes were positive on both sides. An endaural approach surgery was performed under general anesthesia and the cholesteatoma pearl was was peeled off from TM by the help of a curved peak. The pearl shaped mass involved only the outer epidermic layer of the TM without extension into the fibrous layer. After removal, fibrous layer of the TM was intact and myringoplasty was not required. Pathological evaluation of excised material showed that specimen was 0.2 cm in diameter and it was composed of white-yellow granular material. All submitted tissue was processed. Histopathological evaluation showed that submitted tissue was composed of keratin fragments and fibrous granulation tissue. Histological features were compatible with cholesteatoma (Figure 2).
At the 6 month follow up, otoscopic examination was normal with no recurrence. Tympanograms were type A bilaterally and patient had no complaints. DiscussionCongenital cholesteatoma was first described by House in 1953 [9]. Unlike acquired cholesteatomas, the middle ear congenital cholesteatoma is usually identified behind an intact, normal-appearing TM. The patient often has no history of recurrent suppurative ear disease, previous otologic surgery, or TM perforation [10]. The incidence of ME congenital cholesteatoma comprises 2% to 5% of all cholesteatomas [8]. Several theories have been postulated on the pathopyhsiology of congenital cholesteatomas. The 'epithelial rest' theory supports persistance of an epidermoid formation (derivative of the first branchial groove) that normally regresses after 33rd week of gestation [11]. The 'metaplasia theory' postulates that inflamed middle ear mucosa transforms into startified squamous epithelium [12]. Middle ear cholesteatomas might be explained by these theories, but TMCs can not. According to Atmaca et al [8], TMCs may best be explained by Ruedi's theory, in which he postulates that small inflammatory injuries to the TM in utero cause small perforations in the epithelium through which the basal epithelial squamous cell layer proliferates into protruding cones [13]. If these cones retain within an intact TM, TMCs could then be formed. Our case also can best be explained by Ruedi’s theory since only the epithelial layer of TM is involved with spared fibrous layer. Early diagnosis and treatment of TM congenital cholesteatoma is essential to avoid progressive destruction in the ear. A whitish spot on the TM should raise suspicion for cholesteatoma. In differential diagnosis, tympanosclerosis, foreign bodies, keratosis obliterans and cholesterol granuloma always should be kept in mind [14,15]. Especially in children, TM cholesteatoma does not initially cause hearing loss [2]. If remained untouched, they can cause several complications such as ossicular involvement and subsequent hearing conduction impairment similar to any other cholesteatoma of the middle ear. In addition, as the disease stage become advanced, the frequency of the invasion to the epitympanum, hypotympanum, sinus tympani, facial recess, facial canal and the dura is increased [16]. In our case; early diagnosis of congenital TM cholesteatoma provided easy removal of the disease with an intact membrane remained and also avoided more invasive surgery and related complications which might have occured in the future. Although recurrence of TMC is less frequent than middle ear cholesteatoma [17], these lesions may also potentially involve the ossicles and middle ear [11,15]. For this reason, postoperative follow-up is essential. Our patient showed no recurrence in post-operative 4 months period. References
|
|||||
| Keywords : Keratinoz kist , Kolesteatoma , Konjenital kolesteatoma , Timpan Membran , Pediatrik kolesteatoma | |||||
|