|
|||
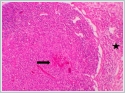
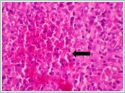
AbstractKikuchi Fujimoto disease is a rarely seen disease of an unknown etiology. It is characterized by fever, neutropenia, elevated erythrocyte sedimentation rate and histiocytic necrotizing lymphadenopathy. It is more common among young Far-East Asian women and occasionally seen in our country. The exact diagnosis of the disease is based on histopathological evaluation of a lymph node biopsy. In this report, we presented a 23 years-old woman with cervical lymphadenopathy with an exact histopathologic diagnosis of Kikuchi Fujimoto disease and reviewed the literature to create a better awareness of the disease for the clinicians.IntroductionThe Kikuchi-Fujimoto disease (KFD) also known as histiocytic necrotizing lymphadenitis is a rarely seen disorder with an unknown etiology. This self-limited disease is characterized by slight fever, neutropenia and elevated erythrocyte sedimentation rate [1]. The disease was first described in 1972 independently by Kikuchi and Fujimoto et al [2-3]. Typically, It occurs in Far-East Asian women in their late 20 s or early 30 s [4,1] The exact diagnosis of the disease is generally based on the histopathologic findings of an excision biopsy of the affected lymph nodes [5]. Clinically and histologically, KFD mimics high-grade lymphoma and it can be mistaken for the lymphadenitis of systemic lupus erythematosus (SLE), infectious mononucleosis or tuberculosis [5]. Case ReportA 23-year-old woman mainly complained of cervical lymphadenopathy (LAP) presented to the Out-Patient Department of our otorhinolaryngology clinic with a history of a swelling on her right neck for 2 months. According to her expression, the first mass occurred in post-auricular region 6 months ago and it disappeared within 4 months. She didn’t describe any systemic symptom. In physical examination, she had mainly an enlarged, mobile, painless and rubbery lymph node in right posterior cervical region and also some other multiple lymphadenopathies were palpated bilaterally. The other physical examination of the patient was unremarkable. Her Neck-Ultrasound revealed a 13X7 mm lymphadenopathy with a dense cortex and pallid echogenic hilum in right posterior cervical region. Also bilateral multiple LAPs up to 23X9 mm in dimension with echogenic hilum were observed. In complete blood count, there was only a slight anemia (erithtocyte: 11.4). And Erythrocyte sedimentation rate (ESR) was 24. Other biochemical tests and serological tests were in normal range. Also thoracic medicine evaluated the patient. The chest X-ray revealed perihilar opacity of left upper and middle zones, but the thoracic computed tomography was reported as in normal range. The sputum examination for acid-fast bacilli was negative and the Tuberculin test was nonreactive. According to these findings, excisional biopsy was decided and an excisional biopsy of the lymph node in right posterior cervical region was performed. The histopathological evaluation elicits a lymph node with paracortical necrosis which lead the diagnosis of Kikuchi-Fujimoto Disease (Figure 1).
During the routine follow-up of the patient, blood tests were within normal limits however ultrasound images showed up the persistence of the lymphadenopathies, but there was no increase in their size. DiscussionKFD is a mysterious disease of acute or subacute onset, developing in two to three weeks with a self-limited course lasting one to four weeks [6]. The disease typically presents with unilateral tenderness cervical lymphadenopathy in the posterior cervical triangle and usually accompanied by mild fever, night sweats and fatigue. The size of the lymph nodes ranges from 0.5 to 4 cm [6]. The disease especially affects individuals younger than forty years (range 19 months to 75 years) [7, 8]. Although it was believed that there was a female predominance, recent studies showed up 1:1 female to male ratio [6, 9]. Interestingly, our patient complaint of only a painless cervical LAP. She didn’t have any systemic symptom. Laboratory studies are mostly normal. In the blood tests of some patients slight anemia, mildly increased ESR, mild leukopenia or leukocytosis could be seen [6]. In our case, there was only a slight anemia and increased ESR. Although the exact etiology of KFD is unknown, an abnormal autoimmune response to an infection has been accused. Brucella, Epstein-Barr virus ¸Yersinia enterocolitica, Toxoplasma gondii, human herpesvirus type 6 and 8, human T-lymphotropic virus type 1, Entamoeba histolytica are thought to be the leading pathogens which are suspected in the etiology [6,10,11]. In our case, patient had no previous infection history and her serological tests showed no acute or subacute infection status. There is no characteristic appearance of an affected lymph node on ultrasonography, computed tomography or magnetic resonance imaging. The radiological findings could be confused with malignant lymphoma and other nodal diseases accompanied by necrosis such as tuberculosis [6, 12]. Therefore, the basis of the diagnosis of the KFD is done by an excisional biopsy of an affected lymph node. The accuracy ratio of fine needle aspiration cytology (FNAC) is 56.3% [13]. So almost half of the cases, fine needle aspiration is not enough for diagnosis. The characteristic histopathologic findings of KFD include paracortical necrosis, abundant karyorrhectic debris with a distortion of nodal architecture and large numbers of different types of histiocytes and plasmacytoid monocytes at the margin of the necrotic area [6,8]. The immunophenotype of the disease exhibit T-bet-expressing CD4 cells accompanied by T-bet-positive CD8 and B cells [14]. Because of a self-limited course of the disease in several weeks to 6 months, treatment is not required in most of the cases. However, the patients with severe symptoms or recurrence of the disease should be treated with systemic corticosteroids [15]. In this case, the patient followed up without any treatment. The KFD might be an under-diagnosed entity especially in patients without a significant systemic symptom just like our patient. In differential diagnosis of patients with fever, unilateral cervical adenopathy, KFD should be kept in mind. References
Presented at16. Rhinocamp KBB ve Rhinocamp Aile Hekimliği Kongresi'nde poster olarak sunulmuştur. |
|||
| Keywords : Histiositik Nekrotizan Lenfadenit , Servikal lenfadenopati , Kikuchi-Fujimoto Hastalığı | |||
|