|
|||||
AbstractProliferating trichilemmal tumors are rare cutaneous malignancies mostly seen in scalp of elderly women. The most important histological feature is trichilemmal calcifications to differentiate them from squamous cell carcinoma. Since their clinical features and follow-up period is different from squamous cell carcinoma, accurate diagnosis must be made for definitive treatment. We presented a case of recurrent proliferating trichilemmal tumor in a 62 years old woman after 9 months of first diagnosis. The first surgery was performed in another institution; tumor was misdiagnosed as squamous cell carcinoma. We discussed the way of treatment and differential diagnosis with current literature.IntroductionProliferating trichilemmal tumor (PTT) is a cutaneous malignancy arising from the outer root sheath of hair follicle [1]. Since it was first reported by Wilson-Jones in 1966 [2] as proliferating epidermoid cyst, different synonyms have been used such as trichilemmal pilar tumor, pilar tumor of scalp, proliferating trichilemmal cyst and PTT [3]. Although almost 50 years after the first diagnosis of a PTT, there is still debate about their malignant potential and biological behavior. Tumor with a totally benign histopathological characteristics may metastasize and malignant pathological features does not always prevent a favorable prognosis [4]. The tumor can be misdiagnosed as squamous cell carcinoma(SCC) and the most important hallmark of the lesion is trichilemmal calcification for differential diagnosis [4]. We presented a case of recurrent PTT, who was misdiagnosed as SCC and treated in this manner. We discussed the importance of differential diagnosis in this rare malignancy under the light of current literature. Case ReportSixty-two years old female patient admitted to our Otorhinolaryngology department for a recurrent scalp lesion. She had a history of SCC in the same region treated with wide local excision 9 months ago. She had no chronic sunlight or occupational chemical exposure history. On her physical examination there was a 3x3 cm. nodular exophytic fungating mass on left side of the occipital region of the scalp (Figure 1).
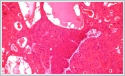
Since preoperative diagnosis was a recurrent SCC, a 18-FDG-Positron emission tomography(PET) was performed for systemic metastasis. There was an intense FDG uptake( SUV max=13.9) in the tumoral mass of the scalp and there was no systemic or regional lymph node metastasis. The tumor was totally excised with 1 cm. safe margins under general anesthesia. In the postoperative pathological examination of the tumor there was interconnecting squamous epithelial cell islands showing trichilemmal keratinization and calcification preoperties (Figure 2).
The postoperative diagnosis was well consistent with proliferating trichilemmal tumor with benign histopathological features. Since the pathology of the second surgery was different from the first; pathological investigation of the first surgical specimen was also done in our institution and histopathological examination of this first malignancy also showed similar features with second surgery. In the postoperative period the patient was free of tumor recurrence after one year of control. DiscussionProliferating trichilemmal tumor is mostly described as a well-circumscribed dermal or subcutaneous neoplasm with squamoid cytological features and trichilemmal keratinization. The most striking histological feature is the potential of this rare malignancy to be misdiagnosed as SCC [5].They are approximately 90% seen in the scalp region, they are presenting as smooth, rounded intradermal swellings sometimes with fungating pattern or ulceration, most of the patients are elderly women. With clinical appearance; epidermoid cyst, keratoacanthoma, SCC, pilomatrixoma, sweat gland tumors, cylindiroma, basal cell carcinoma can be thought in differential diagnosis [4]. Our patient was also an elderly woman with a fungating scalp lesion. Exact cause of PTT is not known; they are presumed to originate from the precursor trichilemmal cysts(TCs), but they can also arise de novo [6]. TCs originate from the outer root sheath of hair follicle. Bald scalp region and follicles without non-terminal hair are unlikely to produce these malignancies, they are mostly seen in hair follicle rich areas on the scalp [7]. TCs, PTTs and malignant PTTs are thought to be a spectrum of tumors in a continuum. Adenomatoid TCs turn into epitheliomatous PTTs and carcinomatous malignant PTTs in a stepwise manner [7]. TCs are fully benign tumors, malignant PTTs behave in an aggressive manner with distant metastasis, PTTs are in the midline of these two [4]. Pathway by which a benign TC or PTT turns into malignant formation is not exactly known, but p53 mutation may be an important factor [8]. Histopathological features of PTT include abrupt, glassy, trichilemmal-type keratinization without infiltration of the surrounding structures [5,6]. Squamoid appearance of pilar cells, mild to moderate cellular atypia, common presence of dyskeratotic cells and mitotic activity are also present in PTTs which make them easily misdiagnosed as SCC [9]. Malignant ones have a frankly invasive component, vascular and/or perineural invasion can also be seen [6]. The role of histopathology in predicting the biological behavior of the tumor is conflicting. Ye et al.[5] proposed a histopathological classification. They found that when tumor cells intensely invade dermis with increased atypia and necrosis, risk of local recurrence and distant metastasis increases. Folpe et al.[9] suggested that non-scalp location, recent rapid growth, size greater than 5 cm., infiltrative growth, significant cytological atypia with mitotic activity anticipate an unfavorable prognosis. On the other hands; even PTTs with totally benign features, devoid of cytological or architectural atypia have metastasized and caused mortality in some patients [10,11]. Although Ki-67 or proliferating cell nuclear antigen can help in differentiating malignant PTTs from benign ones, cellular atypia, chromosomal ploidy or morphometric analysis are not reliable markers [1]. Tumor cells usually have high FDG uptake in 18-FDG-PET. This feature can be used for imaging primary tumor and metastatic foci when malignant potential of the tumor cannot be assessed [1,12]. There was also high FDG uptake( SUVmax=13.9) in 18FDG-PET of our patient. There are fundamental differences between PTT and SCC. Firstly; PTT can be differentiated from SCC by abrupt mode of keratinization, trichilemmal differentiation, presence of clear cells with glycogen storage and sharp demarcation from surrounding tissue without infiltration, histopathologically [6]. Regardless of atypia or invasion, most PTT cells exhibit positive staining with monoclonal antibodies against pilar-type keratin polypeptides such as AE13 and AE14 which are absent in SCC, immunohistochemically [4]. UV radiation and sunlight exposure, HPV infection, occupational exposures, scarring dermatoses, chronic wounds including burns are important risk factors for cutaneous SCC cases, but they are not admissible for PTTs [13]. For our patient, there was also no known predisposing factors. Although both tumors are treated surgically with safe margins, metastatic potential of malignant PTT is more than SCC [4]. Near surgery; malignant PTTs must be treated with additional radiotherapy and/or chemotherapy regimens, but there are limitations in their tumor susceptibility to these treatment protocols. CAV chemotherapy regimen ( cisplatin, adriamysin, vindesine) which can be used for advanced SCC cases, has limited beneficial for malignant PTTs. Cisplatin, bleomycin and adriamycin combination also may have no effects for malignant PTT cases [4]. As a conclusion; for long lasting, recurrent cutaneous lesions PTTs must also be thought in differential diagnosis even though the primary diagnosis is SCC. These rare tumors must be well differentiated from SCCs due to their different biological behavior and risk for life threatening malignant transformation and early metastasis. References
|
|||||
| Keywords : Prolifere trikilemmal tümör , Skuamöz hücreli karsinom , Kutanöz malignite , Trikilemmal kalsifikasyon | |||||
|