|
|||||||
AbstractObjective: This paper reports a case of huge epidermoid cyst in unexpected localization mimicking parotid tumor to highlight the difficulty in obtaining a correct diagnosis.Background and Case Report: This case describes a 33-year-old woman who presented with a huge, soft and painless swelling over right parotid region which was progressively increasing in size over five years. Fine needle aspiration was unsatisfactory and Ultrasonography (USG) scan showed right parotid tumor. The diagnosis of epidermoid cyst was made only upon excision of the mass under general anaesthesia. Post operatively, the recovery was good and there was no complication. Conclusion: Though it is extremely rare, preauricular epidermoid cyst should be considered as a differential diagnosis of painless soft parotid swelling. IntroductionThe epidermoid cyst (EC) is a benign cyst and develops from abnormal epithelial components of ectodermal tissue formed during the fetal period (congenital), or implanted epithelium arising after surgery or trauma (acquired) [1]. The several synonyms are epidermal cyst, epidermal inclusion cyst, infundibular cysts, sebaceous cysts, epithelial cysts and keratin cysts [2]. ECs occur in the head and neck region with an incidence of 6,9-7%[3,4]. Primary ECs of salivary glands appear to be very rare and literature search for the past 25 years revealed only very few cases in parotid gland [5]. Due to the diagnosis of an EC in the parotid gland is a very rare entity, it becomes very essential and it could be easily mistaken for a salivary gland abscess, neoplasm, tuberculous lymphadenitis, metastatic node, or other cystic masses [6]. Thus, to prompt diagnosis and confirmation, surgical approach and histopathological examination is necessary. We would like to report a case of a huge preauricular EC as a rare differential diagnosis of a parotid swelling. We also discussed the embriology, clinical features, evaluation and treatment. Case ReportA 33-year-old woman presented to us with a complaint of painless swelling over the right parotid region for duration of five years. The swelling gradually increased in size and there were no episodes of inflammation or infection of the swelling. She had no other swellings present anywhere else in the body. There wasn’t any sign of paresthesia. She had also no significant past medical or surgical history. Examination revealed a spherical 3x2cm swelling over right parotid region, elevating the preauricular skin (Figure 1). On palpation, the swelling was doughy in consistency, non-tender and non-pulsatile. The findings upon facial nerve and mouth and pharynx examinations were normal and natural, with no signs of cervical lymphodenopathy. No additional pathologies were observed in other ear, nose, throat and system examinations. No other traits were observed in his or family history, either. The routine biochemical and hemogram analyses and lung radiography also proved to be normal. Fine needle aspiration for cytology was performed of the swelling which was unsatisfactory. Ultrasonography (USG) of the right parotid swelling showed a well-defined, homogenous, hypoechoic mass at the right parotid gland measuring 3.5x2.5x1.0cm, with no internal vascularity and no evidence of calculi in the duct or glands seen. A differential diagnosis of benign parotic salivary gland lesion was made.
With the above clinical and imaging correlation, surgical resection was subsequently performed. Initially, a right superficial parotidectomy with facial nerve preservation was planned, however intraoperatively, the tumor was noted to be rather superficial, prompting a total surgical excision sufficient. By this, the elliptical incision was extended from the auricula anterior to superior and the resection was performed up to temporal fascia. A cystic mass was revealed and the cyst surface was followed until excision was carried out (Figure 2A,B).
The surrounding skin was adhered to the swelling which was able to be dissected of by meticulous dissection. Despite the non-aggressive surgical approach, the tumor could be entirely resected with preservation of right parotid gland (Fig. 3).
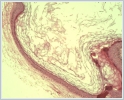
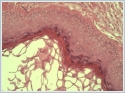
Histopathological examination revealed stratified squamous epithelium with an intraluminal laminated keratinized material confirming the diagnosis of EC in the right pre auricular region (Figure 4 and Figure 5).
Post operatively the healing was uneventful. Patient was discharged day one post operatively with no complication. Patient was well in two years of follow-up with no signs of recurrence. DiscussionThe exact histogenesis of salivary EC is uncertain, but they can be of congenital or acquired type and the most ECs of the skin are acquired. Congenital type is due to failure of surface ectoderm to separate from underlying neural tube in cases of intracranial and spinal ECs but result from entrapment of ectodermal tissue between the midline fusion of first and second branchial arches in the head and neck regions. Acquired type arise from trapped pouches or nearnormal folds of ectoderm, which can be induced by traumatic implantation of the squamous epithelium or obstruction of the duct of a sebaceous gland (pilosebaceous follicle) [7]. Our patient presented no history of surgery or trauma and this would seem to favor the congenital theory. EC of parotid gland is a very rare benign cystic lesion and is seen in young to middle age in adults [8]. Clinically, these cysts manifest as painless, slow-growing, well-circumscribed swellings and without any attachment to the overlying skin or involvement of facial nerve[9]. In the fact that an increased amount of desquamated epithelium or a reaction in the surrounding soft tissue, a sudden enlargement may occurs [10] and this may cause obstruction in salivary duct within the substance of the gland leading to epithelial lining cavity filled with viscous semisolid epithelial degradation product [5]. Cyst also might get infected forming sinus or fistulas if it stays for longer time [11]. Our case presented as swelling mass in preauricular area and clinical signs of infection were not present. ECs are characterized by stratified squamous epithelial lining containing desquamated keratin contents, occasional cholesterol clefts, and foreign body reaction around cyst believed to be due to spillage of cyst contents. The cyst wall consists of a narrow zone of compressed fibrous connective tissue that is generally free of inflammation [11]. The case presented here as an EC wall lined by stratified squamous epithelium containing lamellated keratin without dermal tissues defined. There is always a difficulty of making a correct diagnosis in determining the benign or malignant processes of these lesions. In case of a rapid enlargement with associated lymphadenopathy or facial nerve paralysis, malignant lesions are suspected frequently [2,12]. Additionally, there are reports in the literature of malignant changes in epidermoid cysts[13]. Specialized imaging examinations such as USG, computed tomography, Magnetic Resonance Imaging and histopathological examination should be carried out to provide a correct diagnosis and to develop correct surgical strategy [14]. In our case, there was no lymph node involvement or facial nerve paralysis. Malignant conditions ruled out through meticulous physical examination and USG. Hystopatologic examination of the specimen showed no malignancy. The prognosis of ECs are fairly good and recurrence is very rare. Surgical excision is the only effective treatment for ECs where it is recommended to remove as much of the capsule of the cystic contents, so that it reduces the risk of recurrence [15]. In the current case, total excision was achieved without major complications or by employing preauricular access under general anestesia. In conclusion, though it is extremely rare, ECs should be considered as a differential diagnosis of painless soft parotid swelling. Computed tomography scan might assist in differentiating a huge EC which mimics a parotid tumour. Complete excision is considered necessary to prevent recurrence. Abbreviations: EC, epidermoid cyst, USG, Ultrasonography Financial support and sponsorship: Conflicts of interest: There are no conflicts of interest. Patient consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. Authors’ contributions: ASA was the principal author and major contributor in writing the manuscript. NU performed the histological examination of the epidermoid cyst. All authors reviewed and approved the final manuscript. AcknowledgementWe thank Hilal Kayahan for her help in English revising on this manuscript. References
|
|||||||
| Keywords : Epidermoid kist , preauriküler , parotis bezi , tümör | |||||||
|