|
|||
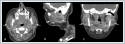
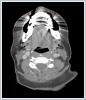
AbstractDilatation of Stensen’s duct usually occurs with obstructive ductal pathology; however, congenital dilatation of Stensen’s duct (CDSD) without an underlying obstructive cause is rarely seen. The case with the congenital dilatation of bilateral Stensen’s and Wharton’s ducts was presented as a first case report in the English literature. A 46-year-old female patient with a painful swelling on the right cheek was admitted to our clinic. She has an episodic swelling on the bilateral cheek that relief with massage for a long time in her medical history. Obstructive pathologies were excluded via sialendoscopy. Computed tomography revealed the bilateral dilated Stensen’s and Wharton’s ducts. We suggested that future studies must uncover the underlying intrauterine causes related to the development of the salivary ductal system for this rare entity.IntroductionDilatation of the Stensen’s duct mostly occurs due to obstructive ductal pathology including sialolithiasis, stricture, mucous plaque and anatomical abnormalities [1]. Dilatation of the Stensen’s duct caused by non-obstructive ductal pathology is rarely seen. The patient with congenital dilatation of Stensen’s duct (CDSD) is usually asymptomatic. Occasionally, the patient with the CDSD has a sialadenitis, and swelling of the cheek on the affected side [2]. Etiology of the CDSD is not fully known; therefore, the genetic background may be a primary role [3]. To the best of our knowledge, Wharton’s duct pathology accompanying the CDSD has not been published, yet. We presented the first case with the dilatation of bilateral Stensen’s and Wharton's ducts. Case ReportA 46-year-old female patient was admitted to painful swelling on the right cheek. The history of the patient had a right sialadenitis of the parotid gland treated with antibiotics five years ago. Before the first sialadenitis of the parotid gland, she had a bilateral episodic swelling on the cheek unrelated to feeding. She denoted that compressing and massaging on the swollen area along the course of the Stensen’s duct had decreased the swelling, although complete remission cannot be achieved. A 12-mm-diameter, hypoechoic and cystic lesion was revealed on ultrasonography (USG) of the right parotid gland. On contrast-enhanced neck computed tomography (CT), bilateral Stensen’s ducts were dilated throughout the entire courses with thickened and enhancing walls. In addition to increased enhancement in parotid parenchyma, intraglandular cystic dilatation of parotid ducts, and bilateral dilatation of proximal Wharton’s ducts were also noted. Sialolithiasis in Wharton’s and Stensen’s ducts was not detected (Figure 1-2).
The sialadenitis of the parotid gland was treated with intravenous ampicillin-sulbactam. After the antibiotherapy, diagnostic sialendoscopy was performed for examination of the ductal wall and excluding obstructive ductal pathology such as stenosis, stricture and radiolucent sialolith. No obstructive pathology was seen during the sialendoscopic procedure, and only dilatation was seen in the right Stensen’s duct. As a result of radiologic and sialendoscopic procedures, the CDSD was diagnosed regarding the Wang’s criteria [4]. Surgical treatment was suggested for recurrent sialadenitis of the right parotid gland but refused by the patient due to the risk of facial paralysis. No complaint and additional sialadenitis attack have occurred during the follow-up period of a year. Written informed consent was obtained for this case report from the patient. DiscussionThe characteristic symptoms of the CDSD are unilateral or bilateral, unrelated to feeding cheek swellings across the Stensen’s duct which mostly decrease with massage, but complete resolution cannot be achieved [5,6]. Etiology of the CDSD is unclear. In the presented case, the dilatation was observed in all of the main salivary ducts. USG, sialography, CT, and sialendoscopy are used for diagnosis of the CDSD. USG of the parotid gland shows an echoless area which corresponds to the dilated Stensen’s duct. Also, it is useful to exclude the obstructive pathologies such as sialolithiasis [7]. Sialography of the parotid gland defines the shape of the dilated Stensen’s duct. It is mostly seen tube-like and well-defined in the CDSD, whereas it gives a sausage-like appearance in the chronic obstructive sialadenitis on the sialography. On the other side, it may be dilated or completely normal [2,8]. Also, CT provides information about ductal dilatation and inflammatory changes in the gland and exclusion of the obstructive sialadenitis caused by sialolithiasis. The appearance of the dilated Stensen’s duct was described as the “Mustache sign” in CT imaging [2]. Addition to the CT, the exclusion of the obstructive causes including radiolucent sialolith, ductal stenosis and stricture were performed by diagnostic sialendoscopy in the present case. We considered that sialendoscopy might be used for the diagnosis of the CDSD if it is available. The etiology of the CDSD is unknown. Hereditary causes or additive dilative effect of ascending infection from the oral cavity and salivary retention to a congenital defect of Stensen’s duct are presumed to be the contributing factors [4]. Since the acquired form of Stensen’s duct dilatation can be seen in obstructive pathologies, the diagnosis of CDSD should be made according to Wang’s criteria [4]. In the present case, the diagnosis of the CDSD was made by the CT, and diagnostic sialendoscopy revealed no obstructive pathologies. Incidentally, asymptomatic bilateral Wharton’s duct dilatation was also seen on the CT. Since the patient had no complaints regarding submandibular glands, sialendoscopy of the Wharton’s ducts was not performed. The coincidental finding of bilateral Wharton’s ducts dilatation in our case may reveal that CDSD has an underlying intrauterine cause regarding salivary duct system development. Asymptomatic patients with the CDSD may be followed-up with conservative treatment. Surgical treatment is recommended for the symptomatic patients who have cosmetic concern and attacks of sialadenitis. Surgical treatments include superficial parotidectomy with excision of Stensen’s duct and marsupialization of the Stensen’s duct to overlying buccal mucosa via an intraoral approach [4,7,8]. Superficial parotidectomy can provide a complete resolution for the swelling; however, it includes risks such as facial palsy, Frey’s syndrome, injury of the greater auricular nerve [7]. For our case, she refused superficial parotidectomy and is still under follow-up for additional sialadenitis attacks. Bilateral CDSD is a rare disease of the parotid gland. CDSD should be considered the differential diagnosis of the patients who have a painless and unrelated to meal swelling on the cheek. This first case presented the coincidental bilateral Stensen’s and Wharton’s duct dilatation, so additional studies must reveal the underlying intrauterine causes related to the development of salivary glands and ducts for this rare entity. Instead of sialography, sialendoscopy may be preferred as a less invasive and radiation-free diagnostic technique for the exclusion of obstructive ductal pathology. References
|
|||
| Keywords : Stensen kanalı , Wharton kanalı , konjenital , dilatasyon | |||
|