Abstract
Liposarcomas (LS) are the most common malignancy of the soft tissue sarcomas. These tumors are most frequently documented in lower extremities and retroperitoneum. Liposarcomas that located in head and neck region are exceedingly rare. Intraoral liposarcomas represent majority of all head and neck liposarcomas. Atypical lipomatous tumor (ALT)/well differ¬entiated liposarcoma (WDLS), which is the most frequent subtype of LS, is associated with better prognosis. Because ALT/WDLS mostly manifests at lower grade and stage at the time of diagnosis. In addition, appropriate surgical excision is the standard suggested curative option. A 34-year-old woman presented with swelling on the right side of the buccal region. She was histopathologically diagnosed with well-differantiated liposarcoma. The tumor has been completely removed and no other adjuvant radiotherapy was applied. We recommend complete surgical resection of liposarcomas without vascular involvement.
Introduction
Sarcomas, which originate from mesenchymal cells, comprise only 1% of all malignancies [1]. Liposarcomas are the most frequent soft tissue sarcomas, accounting for the 20% of all sarcomas. Liposarcomas typically localized in the extremities and the trunk, particularly in retroperitoneum [2]. Furthermore, head and neck sarcomas represents approximately 1% of all head and neck cancers [3]. In addition liposarcomas most commonly detected in cheeks/ buccal mucosa and the tongue. Liposarcoma in head and neck area usually presents at the mean age of 40 years and occur more frequently in male gender. LS is classified into four subgroups; ALT/WDLS, dedifferentiated liposarcoma (DDLS), myxoid liposarcoma, and pleomorphic liposarcoma [4]. ALT/WDLS is the commonly identified subtype, and mostly localized in retroperitoneum. Oral ALT/WDLS typically manifests as a painless, slowly enlarging submucosal masses. Due to the superficial location, asymptomatic lesions are generally small in dimension at the time of diagnosis. Thus they may not detected until they cause any functional and/or cosmetic problem. Magnetic Resonance Imaging (MRI) plays a prominent role in staging of head and neck malignancies. MRI provides valuable diagnostic data through T2 weighted section for examine soft tissue malignancies. The final diagnosis should based on histopathological examination of excisional biopsy sample. Complete surgical excision is the standard suggested curative option for ALT/WDLS. Studies demonstrated that chemoradiotherapy in addition to surgical therapy has been beneficial only for the myxoid subtype [4]. Incomplete surgical excision represents the most frequent cause of local recurrence with a rate of 30%. Although postoperative radiotherapy found to be beneficial in some selected cases, adjuvant chemotherapy is not a curative option.
Case Report
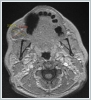
A 34-year-old woman presented with swelling on the right side of the buccal region. A lobule contoured hypoechoic solid nodule with blurred margins of 35*30 mm diameter adjacent to masseter muscle which detected by USG. CT screening revealed hypodense lesion with well-defined margins and 35*30*15 mm diameter in the anterior part of right masseter muscle which extending to the pterygopalatine fossa (Figure 1,2).
Imaging findings strongly indicated an adipose tissue, thus it was decided to remove. Therefore, no fine needle biopsy was performed. Lesion histopathologically defined as sclerosing, well differentiated adipose tissue in post surgical period. In addition, the positive CD34 and S-100 staining indicated well-differantiated liposarcoma. The tumor was completely removed and no additional adjuvant radiotherapy required post-operatively (Figure 3).
Discussion
Although the etiology of the liposarcoma remains uncertain, hematomas after possible trauma seems to play important role occurrence of this tumor. Treatment response is associated with tumor localisation and histological type. Studies revealed significantly better 5-year survival rates for patients with head and neck LS than LS localised in exremities and retroperitoneum respectively [5]. Complete surgical excision is the recommended primary treatment for LS, particularly in young patients with low-grade LS and commonly no radiation required. Local recurrence and distant metastasis are major issues in LS-patients with head and neck region. Davis et al. reported overall local recurrence rate of 53% in their study which included 30 patients with head and neck LS [6]. In recent studies, local recurrence was significantly associated with increased lesion size, younger age, male gender and incomplete excision. On the contrary younger age was linked to increased overall survival and also no clear association found with histopathological type and adjuvant therapy [6,7]. The findings related to local recurrence are debated due to limited number of studies in published data. Well-differantiated and myxoid types, which are mostly reported to arise from head and neck region, exhibiting a tendency to local relapse, and rare metastasis. 5-year survival in both types are better than in the round cell and pleomorphic types [6]. In addition, Gerry et al. compared 318 head and neck LSs with 9485 LSs of other regions by using the Surveillance, Epidemiology, and End Results (SEER) database. Researchers concluded that head and neck LSs were less aggressive and had better prognosis than LSs arised from other parts of body. Researchers also noted that lesions were mostly subcutaneous (81%), low grade (70.1%), and in early stage (p < .001). They also highlighted a significantly better overall survival (p < 0.001) than LSs arised from other parts of body [8]. Lymph node involvement and distant metastasis are relatively rare in LS. Davis et al. reported absence of nodal or distant metastasis at time of diagnosis in 30 LS patients with head and neck. During 21 years follow-up 4 patients had distant metastasis [6]. Supportively Nichols et al. reported no nodal or distant metastasis in a 13-year-old boy with LS located buccal mucosa [9]. On the other hand distant metastasis has reported particularly in patients with high grade LS types (dedifferantiated, pleomorphic) [10]. Thus, due to absence of any metastatic lymph node in our patient, no neck dissection has performed.
It was also documented that LS patients treated with only radiation, achieved worse outcomes than surgical resection or surgery plus adjuvant radiation therapy. Moreover, LSs in head and neck region have the advantage of the superficial location than conventional LS. Thus they are able to identify earlier and can treate more successfully by surgical resection [8]. Numerous researches have documented significanly lower local recurrance and increased survival rates in the group treated with excision only or followed by radiotherapy than the group treated with radiotherapy only [6,7,8]. In conclusion, the tumor has been completely removed in our case and no other adjuvant radiotherapy was applied. In accordance with published data, middle-aged female patient showed no recurrence or distant metastasis during 2 years of follow-up period in our study. We recommend complete surgical resection of liposarcomas of head and neck without vascular involvement or distant metastasis.
References
- Cheng, J., Wang, Y., Cheng, A., Wang, L., Tian, Z., Yu, H., ... & Shen, G. (2011). Primary liposarcoma in oral and maxillofacial region. Journal of Craniofacial Surgery, 22(5), 1765-1771.
- Enzinger MF, Weiss SW. Liposarcoma. In: Weiss SW, Goldblum JR, editors. Soft tissue tumors. 4th ed. St. Louis: Mosby; 2001. p. 641–90.
- Potter, B.O.; Sturgis, E.M. Sarcomas of the head and neck. Surg. Oncol. Clin. N. Am. 2003, 12, 379.
- Dei Tos AP, Marino‑Enriquez A, Pedeutour F and Rossi S: Dedifferentiated Liposarcoma. WHO Classification of Tumours of Soft Tissue and Bone. Fletcher C, Bridge J, Hogendoorn P and Mertens F (eds). 4th edition. Lyon, IARC Press, PP37‑38, 2013.
- Enzinger FM, Weiss, SW (1995) Liposarcoma. Enzinger, FM Weiss, SW eds. Soft tissue tumors ,431-466 Mosby St. Louis, MO
- Davis EC, Ballo MT, Luna MA, Patel SR, Roberts DB, Nong X, Sturgis EM. Liposarcoma of the head and neck: The University of Texas MD Anderson Cancer Center experience. Head & Neck: Journal for the Sciences and Specialties of the Head and Neck. 2009;31(1):28-36.
- Nimura F, Nakasone T, Matsumoto H, Maruyama T, Matayoshi A, Maruyama N, Yoshimi N, Arasaki A, Nishihara K. Dedifferentiated liposarcoma of the oral floor: A case study and literature review of 50 cases of head and neck neoplasm. Oncology letters. 2018;15(5):7681-8.
- Gerry D, Fox NF, Spruill LS, Lentsch EJ. Liposarcoma of the head and neck: Analysis of 318 cases with comparison to non–head and neck sites. Head & neck. 2014;36(3):393-400.
- Nichols EM, Mirmiran A, Garofalo MC, Sun CC, Hatten K, Wolf J. Recurrent myxoid liposarcoma of the buccal mucosa in a young boy: a case report and review of the literature. ENT: Ear, Nose & Throat Journal. 2011;90(12).
- Davis EC, Ballo MT, Luna MA, Patel SR, Sturgis EM. S086 Liposarcoma of the Head and Neck: Experience at a Major Cancer Center. Archives of Otolaryngology–Head & Neck Surgery. 2006;132(8):858-.
|