|
|||
AbstractChondromyxoid fibroma (CMF) is an uncommon benign cartilaginous tumor that usually arises from the proximal metaphyseal ends of the long bones, however, CMF arising from the nasal septum is exceptionally rare. Herein, we present a case of a 47-year-old female patient with a CMF of the nasalseptum. The tumor was completely removed with endoscopic surgery and the patient was free of disease for 12 months.To our knowledge, the present case is the first paper reporting endoscopic complete removal of the nasal septum CMF with free surgical margins.IntroductionChondromyxoid fibroma (CMF) is an uncommon benign cartilaginous tumor that usually arises from the proximal metaphyseal ends of the long bones, especially from the tibia and femur [1].The presence of CMF in the head-neck region is a rare entity and has been reported to have a prevalence of 5.4% among all CMF tumors [2]. Maxilla and mandible are the common areas of CMF occurrence in the skull and facial skeleton, nevertheless CMF arising from the nasal septum is exceptionally rare [3-6]. Herein, we present a case of a female patient with nasal septum CMF whose tumor was totally removed with endoscopic surgery. Case ReportA 47-year-old female presented with the complaint of increasing nasal obstruction lasting for three months. The patient had no other symptoms, including nasal discharge, bleeding or headaches, and there was no history of trauma or previous sinus surgery. Physical and endoscopic examination of the nasal cavity revealed a submucosal nasal mass of the nasal septum with left side predominance (Figure 1A). Preoperative computed tomography (CT) showed a 2.4x2.3x1.8 cm size, solitary, well-defined and expansile nasal septum lesion with mild and heterogeneous contrast involvement. According to magnetic resonance imaging (MRI), the lesion was reported as a benign tumor that involved nasal septum cartilage, vomer and perpendicular lamina, extending through the floor of the bilateral nasal cavity (Figure 1B-D).
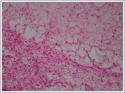
The tumor had a hypointense signal on T1-weighted MRI images, while T2-weighted images showed a hyperintense signal. The patient underwent total endoscopic removal of the tumor with partial excision of nasal septum cartilage, septal mucosa, vomer, perpendicular lamina and left maxilla to establish tumor-free surgical margins. According to intraoperative findings, the tumor was located at the inferior part of the cartilaginous and bony septum junction with partial involvement of vomer, perpendicular lamina and nasal septum cartilage. The tumor was adhered to the septal mucosa bilaterally and was causing slight left maxilla bone erosion in a very limited area. According to frozen section examination, the tumor had cartilaginous and myxoid components without any sign of malignant characteristics including cytological atypia, mitoses or necrosis. Permanent histopathological examination revealed a chondromyxoid appearance with hypocellular lobules, separated by intersecting bands of highly cellular tissue composed of fibroblast-like spindle cells and osteoclasts without any sign of calcification, cytological atypia, mitoses or necrosis (Figure 2). The postoperative course was unremarkable and the patient had no signs of recurrent disease at 12-month follow-up. DiscussionChondromyxoid fibroma was first described by Jaffe and Lichtenstein in 1948 [7].It represents less than 1% of all bone tumors and 1.6% of all benign bone tumors. CMF arises most frequently in males between the age of 20 and 30 years with an additional incidence peak between 50 and 70 years [8, 9].The occurrence of CMF in the craniofacial region was reported for approximately 5% of all CMF cases, occurring slightly later in life than peripheral tumors [2].Meredith et al [6] found the mean age of 21 craniofacial CMF cases to be 44.3 years. The clinical symptoms of CMF in the head-neck region usually depend on the localization of the lesion. In patients with sinonasal CMF, the tumor may not be noticed by patients until it becomes a larger size, similar to other benign tumors of the sinonasal cavity. Nevertheless, a number of symptoms such as nasal obstruction, nasal discharge, bleeding, headache, facial pain and persistent chronic rhinosinusitis may be seen according to the exact location of the tumor [5].In the present case report, the patient was a 47-year-old female with nasal septum CMF and had no symptoms but nasal obstruction. CMF originating from the nasal septum is extremely rare in the literature. To our knowledge, only five cases were reported in the English literature to date, while two of them were presented in a case series composed of 25 craniofacial CMF with no specific data (Table 1) [3-6]. We present an additional case of CMF originating from the nasal septum and, to our knowledge, the present case is the first paper reporting endoscopic complete removal of the tumor with free surgical margins.
Although the majority of CMFs demonstrate well-demarcated tumor margins with a sclerotic rim, cortical thinning or expansion and poorly defined margins with periosteal new bone formation can also be seen in radiological examinations. A purely lucent matrix is a common finding within the tumor, however, a minority of cases can demonstrate mineralization due to microscopic foci of calcific deposits [2].These calcific deposits can rarely be seen in radiological images, in contrast to chondrosarcoma, which has apparent calcifications within the tumor. CMF characteristically shows a hypointense signal with heterogeneous contrast enhancement on T1-weighted MRI examination, while the tumor presents with a hyperintense signal on T2-weighted images [5].In the study of Meredith et al [6]composed of 25 patients with craniofacial CMF, the authors reported that cortical thinning or erosion were common radiological findings similar to those in peripheral tumors, however, unique to the craniofacial region, the tumor had a mainly superficial/exophytic growth pattern from the bone surface. In the present case report, the tumor was a well-defined, heterogeneous and expansile lesion with heterogeneous contrast involvement in CT. MRI examination of the tumor revealed a hypointense signal on T1-weighted images, whereas T2-weighted images showed a hyperintense signal. Calcific deposits were not present within the tumor and these radiological findings agreed to a great extent with the literature. The main histopathological features of CMF are the biphasic arrangement of the myxoid or cartilaginous areas with stellate or spindle-shaped cells with eosinophilic cytoplasm arranged in lobules [2].The tumor may show either a macrolobular or a microlobular pattern and the neoplastic cells are usually encountered at the periphery of the lobules. Tumoral cells in CMF can demonstrate pleomorphism with larger and bizarre nuclei. Mitotic figures are seen very rarely or are absent in CMF, and if present they are mostly located in the hypercellular areas. Microscopic foci of calcification within the tumor can be seen with varied incidence [6]. The differential diagnosis of CMF includes chondroma, chondroblastoma, fibromyxoma, myoepithelial lesions, osteosarcoma and chondrosarcoma. A diagnostic challenge between low-grade chondrosarcoma and CMF may be encountered especially for biopsy materials with limited tissue sampling [4].However, in contrast to CMFs, chondrosarcomas mainly present with a uniform cellular arrangement with well-differentiated hyaline cartilage and the absence of a fibrous component. Surgical resection with tumor-free margins, if possible, is the best treatment modality for CMF. Radiotherapy has been proposed for inoperable or recurrent diseases, nevertheless, clinicians should consider the increased risk of malignant transformation within the tumor due to radiotherapy [10]. Wu et al [2] found the recurrence rate of CMF to be 11.5%, whereas it was reported as 33% in a study involving only craniofacial CMFs [6].In the present case report, the tumor was completely removed via endoscopic surgery and tumor-free surgical margins were validated by multiple frozen section studies. The patient had no signs of recurrent disease at the 1-year-follow-up. In conclusion, CMF is a benign neoplasm that occurs very rarely in the nasal septum and surgery is the most preferred therapeutic option for treatment of these tumors, as indicated in the literature [3-5]. Although based on the data derived from a single case in our study, complete removal of the tumor with safe surgical margins can be achieved by endoscopic surgery with less surgical morbidity in patients with CMF located at the nasal septum. References
|
|||
| Keywords : Kondromiksoidfibrom , nazal septum , cerrahi. | |||
|