|
|||||||||||
AbstractCongenital jugular phlebectasia is a rare clinical entity characterized by fusiform or saccular dilatation of the internal jugular vein (IJV) without torsion. Typically, it is diagnosed in children with a neck mass and is believed to be congenital in origin. It is more common on the right side of the neck and is twice as common in boys as in girls. These asymptomatic masses become larger with crying, straining, coughing, or the Valsalva maneuver. Venous cyst, venous aneurysm, and jugular venous ectasia are other names given to jugular phlebectasiaIntroductionCongenital jugular phlebectasia is a rare clinical entity characterized by fusiform or saccular dilatation of the internal jugular vein (IJV) without torsion. Typically, it is diagnosed in children with a neck mass and is believed to be congenital in origin. It is more common on the right side of the neck and is twice as common in boys as in girls. These asymptomatic masses become larger with crying, straining, coughing, or the Valsalva maneuver. Venous cyst, venous aneurysm, and jugular venous ectasia are other names given to jugular phlebectasia. Case ReportCase 1 An 18-year-old male first developed a right neck swelling at the age of 7 years while crying. He was admitted to our clinic at age 10 because his family was worried about the swelling. He had no history of surgery or trauma. On physical examination, the patient’s neck was of normal size during rest (Figure 1), but a 3×4-cm, smooth surfaced, painless, soft viscous mass was detected at the anterior aspect of the right sternocleidomastoid muscle (SCM) on coughing (Figure 2).
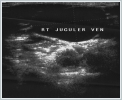
The patient did not describe pain, difficulty swallowing, or loss of consciousness. No murmur or thrill was detected over the mass. Neck ultrasonography (USG) and Doppler ultrasonography (DUSG) showed no difference at rest (Figure 3), but during a Valsalva maneuver, the right IJV appeared ectatic and dilated (Figure 4).
Contrast-enhanced neck computed tomography (CT) showed a markedly ectatic IJV that was markedly dilated during the Valsalva maneuver. Neck magnetic resonance (MR) venography (Figure 5) showed that the right jugular vein was dominant and wide compared with the left. The remainder of the patient’s physical examination and laboratory tests were normal. No pathological condition has been observed during 8 years of follow-up.
Case 2 A 17-year-old male was first brought to our clinic complaining of a swelling on the right side of the neck that developed while crying when he was 5 years old. A soft viscous, painless, widespread mass was observed on the anterior aspect of the right SCM during the Valsalva maneuver and disappeared at rest. A physical examination and plain radiographs taken at the time were normal. Direct laryngoscopy produced normal results. Marked dilatation and increased venous flow was observed in the right IJV on neck DUSG. Contrast-enhanced neck CT and cervical MR venography were performed. No problems have been observed during 12 years of follow-up. DiscussionGerwig [1] first used the term phlebectasia to describe abnormal fusiform dilatation of a vessel in 1952. Phlebectasia is an asymptomatic, unilateral, soft, pulseless, non-tender mass often involving the IJV that expands with increased pressure, crying, sneezing, coughing, or the Valsalva maneuver. It can involve the internal or external jugular vein, mainly the IJV, and occurs predominantly on the right side of the neck [1–4]. The etiology of jugular phlebectasia is uncertain; abnormal enlargement of the IJV, increased tone of the anterior scalenus muscle, compression of the jugular vein between the clavicle and right lung cupula, radiation of the superior mediastinum, trauma, and congenital causes are the most commonly proposed etiologies [4–7]. Jugular phlebectasia is diagnosed easily with a detailed history, physical examination, and imaging methods. It can be also diagnosed with invasive contrast-enhanced radiography or surgical exploration. Currently, DUSG, USG, venography, arteriography, angiography, contrast-enhanced CT, and MR imaging are the most commonly used noninvasive imaging modalities in the diagnosis of jugular phlebectasia; these methods are as accurate as invasive radiological studies and surgical exploration [7]. Although cystic masses of the neck are included in the differential diagnosis, internal jugular phlebectasia is usually confused with a laryngocele enlarging with the Valsalva maneuver, hyperinflation of the lung cupula, and upper mediastinal tumors and cysts [8,9]. Lifetime follow-up appears to be sufficient instead of surgical treatment [2,3,8–10]. Balık et al. [3] suggested surgical intervention because of the risk of thrombosis and cosmetic problems. We did not consider surgical intervention since both of our patients were still growing and did not have any complaints other than neck swelling appearing with straining and crying, so we decided to follow them conservatively. Histopathological studies of surgically removed specimens showed normal dilated veins in most cases [2,5,8,11], although congenital defects or changes in the muscular layer of the vein wall were found in some specimens [2,9–11]. Leighton et al. [2] removed the phlebectasic part of the IJV surgically for treatment and observed smooth muscle fibers arranged randomly on the vessel wall and fat tissue islets extending to the tunica intima between the fibers. They called the phlebectasia a vascular hamartoma. The most important complication of jugular phlebectasia is spontaneous or traumatic rupture of the vein. Therefore, it is important that the patient protect himself/herself from trauma. Some studies advocate surgical treatment for jugular phlebectasia due to the risk of rupture [11]. The development of thrombosis and phlebitis should also be considered when treating jugular phlebectasia [2,3,8]. In conclusion, phlebectasia should be included in the differential diagnosis of atypical neck masses. It can be diagnosed easily with a detailed history and physical examination. USG should be the first choice for diagnostic tests. After the diagnosis is made, the patient should be followed regularly and the patient and his or her parents (for a child) should be informed about the risk of complications such as hemorrhage, infection, and thrombosis. Most importantly, the patient should be comforted that his/her daily life will not be affected. References
|
|||||||||||
| Keywords : Juguler ven , Flebektazi , Boyunda kitle | |||||||||||
|