|
|||||
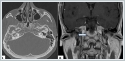
AbstractMiddle ear adenomas are generally benign tumors and are thought to be originated from the middle ear mucosa. MEAs are rare tumors and the frequency between all middle ear tumors is about 2 %. We prepared this report by discussing a case that we encountered with a different intraoperative diagnosis in a patient who underwent surgery for middle ear pathology.IntroductionMiddle ear adenomas (MEAs) are rare tumors and its frequency between all middle ear tumors is about 2 %. MEAs are generally benign tumors and are thought to be originated from the middle ear mucosa [1]. The tumor which can have neuroendocrine differentiation capacity has previously been described in the literature under different names; cerminoma, ceruminous adenoma, monomorphic adenoma, adenocarcinoma, carcinoid tumor etc. In recent studies, it was found that all these tumors have same origin with different degrees of differentiation and were joined under the name of neuroendocrine adenoma of the middle ear (NAME) [2]. In this report, we wanted to increase autologists' awareness on this issue by presenting a MEA case, a rare type of middle ear neoplasm. Case ReportA 42-year-old man presented to our clinic with hearing loss and fullness on the right ear. It was learned that the complaint of hearing loss and fullness in the right ear continued for 4-5 years. He did not report additional symptoms such as tinnitus or dizziness and he had no complaints in the opposite ear. Our patient did not have a systemic disease and did not have the medication he used constantly. At otoscopic examination, retrotympanic effusion and fullness was observed,tympanic membrane was intact but discolored. At pure tone audiometry, bone conduction/air conduction was 12/37 decibel (dB) in right ear and also type B tympanogram was detected. At Computed Tomography (CT) examination a soft tissue density was observed in the mastoid cells, epitympanium and Prussak’s space (Figure 1A). There was no diffusion limitation and no mass lesion in Magnetic Resonance Imaging (MRI) (Figure 1B). With these results, it was decided to perform surgery with an exploration plan.
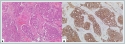
When entered into the middle ear after tympanomeatal flap elevation with the endaural incision, a polypoid, well-defined mass, which is surrounding incus and incudomalleolar joint, was found. No free fluid was encountered in the mastoid cavity and middle ear cavity. The mass was totally excised by canal wall-up tympanomastoidectomy. Pathological examination of the mass was carcinoid tumor of the middle ear (Figure 2).
After operation the patient had no complication or complaints. Since it is a tumor capable of metastasis, Positron Emission Tomography (PET)-CT imaging was performed, but no metastasis was detected in the surgical area and in the distant area. At the pure tone audiogram air-bone gap has fallen to 15 dB at the sixth month examination. DiscussionMEA was first described in two different study in 1976 as 'middle ear adenomatous tumor' by Hyams and Michaels[ ][3] together with Derlacki and Barney[ ][4]. Murphy[ ][5] described that this tumor had carcinoid tumor characteristics and neuroendocrine differentiation in 1980. Many studies have proved that these tumors, which are named with different names, are the same tumor kinds with different glandular and neuroendocrine differentiation levels. Later, Torske[ ][2] called all of these tumors NAME. Saliba and Evrard's[ ][6] classification of NAME which was into three subgroups, according to the immunohistochemical findings and metastatic characteristics, is now the most frequently used classification for NAME. With this classification Type-1 tumors are ‘Neuroendocrine Adenoma of the Middle Ear’ and shows positive immunohistochemistry and negative metastasis. Type-2 tumors named ‘Middle Ear Adenoma’ and they are show negative immunohistochemistry and negative metastasis. Positive immunohistochemistry and positive metastasis and/or carcinoid sydrome showing tumors are Type-3, which named ‘Carcinoid Tumors of the Middle Ear’. The proportions of these tumors were 76%, 20% and 4%, respectively. The most frequent complaints of patients are unilateral hearing loss. Besides, some complaints such as ear fullness, tinnitus, ear pain, vertigo can be seen but some patients could be asymptomatic. At otoscopic examination a retrotympanic mass is observed, but this finding is unclear at most of the patients, or even if the mass is noticed, there isn’t a distinctive feature and color from other middle ear masses. At imaging methods tumor is localized in the middle ear, most of the cases have no bone erosion or invasion. These clinical symptoms and signs are not specific to any disease, which often occurs in other middle ear pathologies. Therefore, many pathologies such as chronic suppurative otitis media, chronic otitis media with effusion, cholesteatoma, schwannoma, teratoma, meningioma, paraganglioma should be evaluated in the differential diagnosis of MEA [1, 7]. Another differential diagnosis of MEA is glomus tympanicum (GT). GT is a special type of paraganglioma located in the middle ear and is the most common primary tumor of the middle ear. GT is included in the differential diagnosis of mea by its localization, symptomatology and malignant potential. On otoscopic examination, GT may appear as a pulsatile red-blue mass. This finding can also be seen in patients with MEA and is not a reliable criterion for distinguishing GT. Digital subtraction angiography is the most important imaging method to be used in the differentiation of these two tumors, which show similar features in CT and MR images. Digital subtraction angiography is the gold standard in the diagnosis of GT and easily distinguishes GT, a vascular tumor, from MEA, an avascular tumor [8, 9]. The main complaint of our patient was hearing loss. Middle ear effusion, conductive hearing loss and type B tympanogram led us to the diagnosis of chronic otitis media with effusion. However, an exploration decision was made because the ear examination did not match the chronic otitis media with effusion exactly and the middle ear mass was suspected on CT and MRI images. Surgery is the first treatment option to MEA. Transcanal approach could be prefer at small-sized tumors, tumors limited to the middle ear, or tumors that enter the external auditory canal beyond the tympanic membrane. Canal wall-up masteidectomy and tympanoplasty should be prefer at tumors extending to the epitympanium or mastoid cavity [10]. In our patient, ossicle chain was partially surrounded by tumor. The tumor was carefully dissected and ossiculoplasty was not needed. There was no invasion of the mastoid cells or facial nerve canal, but canal wall-up mastoidectomy was performed to ensure mastoid cell ventilation. Although Saliba et al.[ ][6] have argued that there is more recurrence in patients without ossiculoplasty, we didn’t reconstruction because we have totally excised the tumor and the ossicle chain is intact. Adjuvant chemotherapy and radiotherapy treatments are usually not used to MEA. Fundakowski et al.[ ][11] have added cervical neck dissection and radiotherapy in patients with lymph node and distant organ metastasis. Ramsey et al.[12] suggest that treatment with parotidectomy or neck dissection should be performed in patients with regional metastasis. It is difficult to comment success of adjuvant therapies at MEA for now.
References
Presented at40. Türk Ulusal Kulak Burun Boğaz ve Baş Boyun Cerrahisi Kongresi , Antalya, Türkiye, 7-11 Kasım 2018 |
|||||
| Keywords : Orta Kulak Adenomu , Orta Kulağın Nöroendokrin Adenomu , Orta kulağın Karsinoid Tümörü , Kanal Wall-up Timpanoplasti , Pozitron Emis | |||||
|