|
|||||||||
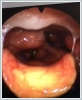
AbstractLymphomas are malignant masses arising from lymph nodes and other lymphatic tissues. Primary lymphoma of the larynx is extremely rare, accounting for less than 1% of all primary laryngeal neoplasms. Classical symptoms of laryngeal lymphoma include lymphadenopathy, dysphagia, hoarseness, and shortness of breath, and systemic symptoms are less common. In this case report, we tried to draw attention to the clinical features of laryngeal lymphoma by reporting a case, which at first glance looks like laryngeal SCC and is located in an area that can be called atypical.IntroductionLymphoma is malignant mass arising from lymph nodes and other lymphatic tissues. Although there are many subtypes, the disease is generally divided into two main groups as Hodgkin and Non Hodgkin lymphoma (NHL). NHL can also be seen in extranodal regions, the head and neck (salivary gland, larynx, nose and paranasal region, etc.) is the second most common site of NHL. It is more common in men than in women [1,2]. In the larynx, it is usually involved in the supraglottic region [3]. Among malignant tumors of the larynx, squamous cell carcinoma (SCC) is the most common pathological type, while primary lymphoma of the larynx is extremely rare. It accounts for less than 1% of all primary laryngeal neoplasms [4]. Classical symptoms of laryngeal lymphoma include lymphadenopathy, dysphagia, hoarseness, and dyspnea, and systemic symptoms are less common [5]. In this case report, we tried to draw attention to the clinical features of laryngeal lymphoma by reporting a case of laryngeal lymphoma, which at first glance looks like laryngeal SCC and is located in an area that can be called atypical. Case ReportAn 84-year-old male patient was admitted to our clinic with the complaint of hoarseness that persisted for more than two months. The patient also had complaints of cough and dysphagia. The patient did not have complaints such as fever, night sweats, insomnia or weight loss. The patient had no history of smoking and alcohol consumption. His history was unremarkable except for prostatic hypertrophy. Neck examination revealed palpable lymphadenopathy in the right submandibular region. In the flexible laryngoscopy, a smooth-surfaced submucosal mass extending from the right pyriform sinus to the vocal cord was detected (Figure 1). Contrast-enhanced magnetic resonance imaging (MRI) of the patient showed well-defined homogeneous contrast enhancement with dimensions of 32x12 mm, extending from the supraglottic level to the pyriform sinus. The lesion was found to have signaling properties similar to lymph nodes in the neck. It was observed that the right pyriform sinus was obliterated due to the lesion (Figure 2).
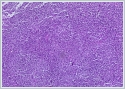
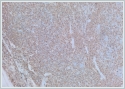
It was decided to take biopsy from the patient by direct laryngoscopy. In the immunohistochemical examination of the biopsy, atypical lymphoid cells showed diffuse expression with CD20 and Bcl-2, focal positivity with CD5, and small patch positivity with CD10 and Bcl-6.(Figure3-4) Reactive staining was observed with T cell markers CD3 and CD2. Since it suggested mature B-cell lymphoma as a result of immunohistochemical evaluations, it was suggested to perform an excisional biopsy from the lymph node in the neck for a definitive diagnosis. As a result of the excisional biopsy, the patient was diagnosed with low-grade B-cell marginal zone lymphoma.
DiscussionThe most common extranodal head and neck regions of primary NHL are the paranasal sinuses, salivary glands, and thyroid gland [2]. Since the laryngeal region contains less lymphoid tissue compared to other areas in the respiratory tract, lymphomas of this region are observed less frequently [6]. NHL is presumed to originate from two locations within the larynx; predominantly from B-cell-derived clusters of specialized lymphoid tissue in the submucosa or from mucosal-associated lymphoid tissue (MALT) in the aryepiglottic folds and epiglottis [7]. The most common site of development of primary laryngeal lymphomas is the supraglottic region. In our case, the laryngeal lymphoma was MALT type and extended from the supraglottic region to the pyriform sinus. Mucosal-associated lymphoid tissue lymphoma occurs in extranodal, mucosal lymphoid tissue and represents up to 7.6% of all lymphomas. In contrast to low-grade nodal B lymphomas, which generally spread at the time of diagnosis, its spread is more limited [8]. The most common locations are the mucosa of the gastrointestinal tract. However, they can also occur in the lungs, salivary glands, skin, and other areas, including the thyroid. It is thought that mucosa-associated lymphoid tissue lymphomas develop from lymphocytic tissue acquired during a chronic inflammatory or autoimmune process [6-8]. In our case, however, no chronic inflammatory diseases were found. In laryngeal lymphoma cases, endoscopic examination usually shows a smooth, polypoid or submucosal mass, ulcerated lesions are rarely observed. The mean age at diagnosis of the patients is reported as 70, and the male/female ratio is different in many series [9]. Although imaging techniques such as computed tomography and MRI can be helpful in the evaluation of any laryngeal neoplasm; definitive diagnosis is made by biopsy [7]. Primary laryngeal lymphoma is more commonly of B-cell origin, but T-cell and NK-cell lymphomas have also been reported and are more difficult to diagnose, often requiring deep and sometimes repeated biopsy [10]. Today, lymphoma treatment is based on an integrated medical approach that combines chemotherapy, radiotherapy, immunotherapy, and surgery. Chemotherapy and radiotherapy are the most common therapeutic strategies for the treatment of laryngeal lymphomas. The prognosis of laryngeal lymphoma depends on many factors, including an accurate biopsy, presence of B symptoms, cell type, gender, staging, lymph node involvement, and response to therapy. Therefore, individualized treatment is advocated in the treatment of laryngeal lymphoma [11]. ConclusionIn this report, we presented a case of a patient who presented with a laryngeal mass, and performed direct laryngoscopic surgery with the prediagnosis of metastatic laryngeal SCC. As a result of the biopsies, the patient was diagnosed with B-cell marginal zone lymphoma. In this case, we tried to draw attention to the possibility of rare diagnostic lesions in a patient presenting with a laryngeal mass. Informed consent was obtained from the patient for this report. Informed Consentfrom the patientReferences
|
|||||||||
| Keywords : Larinks , Lenfoma | |||||||||
|