|
|||||||||||||
AbstractNecrotizing fasciitis is a rare, progressive and life-threatening bacterial infection which spreads with frightening speed along the fascial planes and subcutaneous tissue resulting in extensive tissuenecrosis and often death. Rapidly spreading necrosis often causes systemic sepsis, toxic shock syndrome and multiple organ failure. The origin is generally odontogenic or pharyngeal, involving a mixed flora of microorganisms. Descending infection and mediastinal involvement are usually associated and are the main complications. Factors affecting the success of the treatment of necrotizing fasciitis are early diagnosis, appropriate antibiotics and surgical debridement. This article is presented in a diabetic patient with necrotizing fasciitis of the neck originated from odontogenic infection. Clinical features, pathogenesis and treatment of the case are discussed with the literature IntroductionNecrotising fasciitis (NF) is a rare and life-threatening infection which spreads along the fascial planes and subsequently causes necrosis of subcutaneous fat, skin and sometimes muscle. Infection primarily involves the superficial fascia and progresses into surrounding tissues; progress is often fulminant and may involve all soft-tissues components [1]. Necrotising fasciitis occurs more commonly in patients with compromised immune systems, and more frequently in the abdominal wall, perineum, and extremities [2]. NF rarely involves the head and neck region; and if it occurs, it is usually due to the spread of infection from the teeth or pharynx [3]. Cultures from cervical necrotising fasciitis with a dental source are more likely to include anaerobes, whereas cases associated with pharyngeal mucosa or skin trauma more likely include Staphylococcus and Streptococcus species [4,5]. Cervical necrotizing fasciitis caused by Klebsiella pneumoniae, however, is a rare entity. Necrotizing fasciitis of the head and neck has a particularly high mortality rate due to the proximity of many vital anatomical structures. Known complications of cervical necrotizing fasciitis include airway compromise, arterial and venous occlusion and the extension of infection into the mediastinal and pleural spaces [6]. Treatment of the disease is early diagnosis, a careful aggressive debridement, parenteral antibiotic treatment, and supporting treatment controlling an underlying preparative, and aggravating factors. Case ReportA 75 year old male with known history of diabetes mellitus presented to Bulent Ecevit University, Otorhinolaryngology – Head and Neck Surgery Department with a history of progressive neck swelling and dysphagia for one week. On examination, he was drowsy and dehydrated with poor oral hygiene and no evidence of respiratory compromise. He demonstrated swelling and tenderness over the right neck extending sternal notch (Figure1). Palpation revealed crepitation on right side of the neck region. On physical examination right lower molar teeth decay was noticed. Indirect laryngoscopy was performed to evaluate the airway status. On indirect laryngoscopy, laryngeal examination was normal and the airway was patent. Other otolaryngologic examinations were normal. Laboratory work was remarkable, with a white blood cell count of 16.6 × 109/L, C-reactive protein (CRP) level of 143 mg/L, and glucose level of 216 mg/dL. Empirical broad spectrum antibiotics (ceftriaxone and metronidazole)were started.
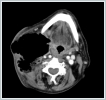
Computerised tomography(CT) scan showed an extensive hypodense collection with air pockets in the right servical region. It was also noted that the extensive collection involves internal jugular vein (Figure 2).
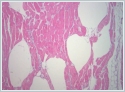
After first evaluation of the patient, the clinical examination and neck ct scan signs were suggested that the diagnosis was necrotising fasciitis on neck. The patient was admitted. Immediate neck exploration and debridement under general anesthesia was planned. Informed consent was obtained from the patient for treatment and surgery. Under general anesthesa, an extensive debridement was done where all the deep fascial planes of the right side of the neck and part of the anterior chest wall was debrided untill there was evidence of fresh bleeding from the skin edges. The right internal jugular vein was found exposed. Necrotic tissues and purulent materials were debride, and the wound was left open (Figure 3). Histologic findings showed gas inclusions between the muscle fibres and subfascial planes (Figure 4). Klebsiella species was isolated from the wound. Klebsiella species was isolated from the wound. Antibiotic sensitivity test showed that isolated Klebsiella species was sensitive to ceftriaxone, gentamicin, ciprofloxacin and trimethoprim/sulfamethoxazole.
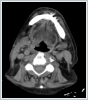
The wound was dressed and debrided daily, and closed with antibiotic gas.The CT scan of the neck showed significant improvement of the infection (Figure 4). The wound granulated well after two weeks and was closed in the event that the wound area epithelised (Figure 5). The patient being discharged on hospital day 14 on oral ciprofloxacin. On the first month after the surgery, the wound was totally healed.
DiscussionNecrotising fasciitis is a severe and potentially fatal infection of the dermal, fascial and subcutaneous layers of the skin. The causative organisms are commonly Group A Beta Haemolytic Streptococci or Staphylococcus Aureus as single agent or may be a polymicrobial infections. Polymicrobial infections are caused by mixed aerobic and anaerobic pathogens. Streptococcus pyogenes (group A Streptococcus ) is the most classic pathogen [7]. Monomicrobial Klebsiella Pneumonia necrotising fasciitis accounted for 11% of all NF cases [8]. Necrotizing fasciitis of the head and neck region is uncommon [9]. In a large series of 128 cases of necrotizing fasciitis, only five of them involved the head and neck region [10]. The commonest cause of cervical necrotising fasciitis is dental infections. Dental infection of the second or third molar teeth may cause cervicofacial infection. This is because the roots of these molars extend below the insertion of the mylohyoid muscle, which is connected to the submandibular space [11]. Immunocompromised patients and patients with sistemic disease such as diabetes mellitus are at an increased risk of developing this infection. Descending infection and mediastinal involve-ment are usually associated and are the main complications [12]. Hsiao et al. reported that the most common symptoms were swelling and pain, which occurred in 71.1% and 54.7% of cases, respectively [10]. Dysphagia and odynophagia are also common symptoms [13]. Our patient was diabetic and had swelling and tenderness over the right neck extending sternal notch. CT imaging is useful in the diagnosis of the necrotising fasciitis. CT characteristics correlate with pathologic findings of soft-tissue inflammation or liquefactive necrosis and thus may feature dermal thickening, increased soft-tissue attenuation, inflammatory fat stranding, and possible superficial or deep crescentic fluid or air in the subfascial planes [14,15]. In our patient, CT scan showed an extensive hypodense collection with air pockets in the right servical region. It was also noted that the extensive collection involves internal jugular vein. MRI is the modality of choice for detailed evaluation of soft-tissue infection but is often not performed for necrotizing fasciitis evaluation because its acquisition is time consuming and will delay treatment [16,17]. The first step of treatment is securing the airway. If the airway is compromised, early intubation or tracheostomy should be considered. Early aggressive surgical intervention with eradication of the source of infection is important. Besides surgical treatment, broad spectrum empiric antibiotics should be initiated. Initial treatment should cover the most commonly involved microorganisms, such as group A Streptococcus and anaerobes,and nowadays is extended to gram-negatives such as Klebsiella Pneumonia and Staphylococcus. However, prior studies of Klebsiella Pneumoniae infection have found no significant association between appropriate empiric antibiotic treatment and outcomes [18,19]. In addition, regular and frequent debridement with appropriate wound dressing is helpful for better outcomes. In this case, after first evaluation of the patient, immediate neck exploration and debridement under general anesthesia was performed. Empirical broad spectrum antibiotics (ceftriaxone and metronidazole) were immediately started. The wound left open and was dressed and debrided daily, and closed with antibiotic gas. After two weeks, the wound healed and the patient was discharged. Informed ConsentHastadanReferences
|
|||||||||||||
| Keywords : nekrotizan fasiit , klebsiella pneumonia , apse | |||||||||||||
|