|
|||||||
AbstractLangerhans cell histiocytosis is myeloid neoplasia that occurs due to abnormal proliferation of histiocytes and can have local and systemic involvement. It is a rare disorder of childhood but also can occur in adults. The male-female ratio of the disease is 2:1. Although the main sites of involvement are skin, bone, and soft tissue, multifocal systemic involvement can occur. Temporal bone involvement is one of the manifestations of the disease. The two most common symptoms of temporal bone involvement are otorrhea and subjective hearing loss. Otalgia and postauricular swelling/tenderness may accompany. Bilateral temporal bone involvement is rare, but there are previously reported case reports in the literature. Most reported cases are in the pediatric age group; the first complaints are usually otorrhea and hearing loss.We present a case of Langerhans cell histiocytosis, who applied to us with the complaint of otalgia and postauricular tenderness in the left ear, and who had bilateral temporal bone involvement on examination. IntroductionLangerhans cell histiocytosis is an idiopathic disease involving the skin, bone, lung, liver, lymph nodes, mucocutaneous tissues, and endocrine organs locally or widely, with the cloning of abnormal histiocytes. Although the disease is usually seen in children, it can also occur in adulthood. Although it primarily affects children aged 1-4, its incidence in children has been determined as 5-6 per million in the United States. Langerhans cell histiocytosis has historically been divided into 3 classes. First is eosinophilic granuloma, a variant with single or multiple bone involvement without visceral involvement. The tumor may resolve spontaneously. It is considered benign. The second is Letterer Siwe's disease, a variant that progresses to multiple granulomas. It can invade the liver, spleen, lymph nodes, and central nervous system and have a poor course. Hand Christian Schuller disease is the last variant. It presents with the triad of multiple bone lesions, exophthalmos, and diabetes insipidus. Schüller firstly described otologic manifestations of Langerhans cell histiocytosis in 1915 [1] . Also, Letterer described a case with a fever, purulent otitis media, lymphadenopathy, and hepatosplenomegaly [1]. Among the main symptoms of otological involvement are ear discharge resistance to medical treatment, hearing loss, swelling, and pain in the mastoid region. The posterior wall of the external auditory canal may erode [2]. The symptoms can be confused with conditions such as cholesteatoma and acute suppurative otitis in different periods of the disease. We present a case of Langerhans cell histiocytosis with bilateral temporal bone involvement, who came to us with the complaint of pain in the left ear.
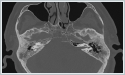
Case ReportA 50-year-old male patient with no known comorbidity and no previous otolaryngological operation was admitted to our clinic complaining of pain in the left ear. The patient indicated that the pain had been going on for a long time and was increasing gradually. There were no complaints of hearing loss or ear discharge. The patient did not have facial paralysis before. In the otoscopic examination, bilateral tympanic membranes were intact, and the external auditory canal was normal. Tenderness was detected on palpation of the left mastoid process. In further evaluation, audiometry and temporal CT examinations were performed. The patient had a symmetric bilateral mild sensorineural loss in pure tone audiometry.(The patient could not undergo a speech discrimination test (SDT) due to their inability to speak the same language as the audiologist and lack of proficiency in English.). Local destructive lesions in bilateral mastoid cells and middle ear were observed in temporal CT (Figure 1).An incisional biopsy was planned. The lesion area was reached with the left postauricular incision. After the skin and subcutaneous tissues were passed, it was observed that the bone tissue expected to be seen was eroded, and a granulomatous lesion protruding beyond it was detected. Biopsy material was obtained, and the result of the histopathological examination was compatible with Langerhans Cell Histiocytosis. A position emission tomography-computer tomography (PET-CT) scan was performed with the oncology opinion. There were lytic sclerotic lesions that involved both temporal bones, with higher FDG uptake in the left temporal bone (SUVMAX: 15.28) compared to the right (SUVMAX: 10.53). (Figure 1).
There was no significant difference in the patient's post-treatment audiometry compared to pre-treatment audiometry. (Figure 4)
DiscussionLangerhans cell histiocytosis is a disease caused by abnormal proliferation of histiocytes, progresses with granuloma formation, and can cause invasion and local destruction. At the same time, it may have a multifocal course and may lead to conditions such as systemic involvement and organ failure [3]. It is seen twice as often in men than in women, and its incidence in adults is rarer than in children [4]. LCH frequently affects the external and middle ear. Still, accurate diagnosis can be challenging due to its clinical presentation. It can be mistaken for more prevalent conditions such as mastoiditis, chronic otitis media, recurrent otitis externa or otitis media, stenosis, or polyps in the external auditory canal. Other less common symptoms include peri-auricular or middle ear masses, conductive hearing loss, otalgia, otorrhagia [9]. Some tumoral formations can also cause destruction in the middle ear. Cholesteatoma is the most commonly seen among them and is considered in the differential diagnosis before LGH. It can be differentiated by diffusion restriction on MRI examination. Glomus tumors (jugular and tympanic) can sometimes be aggressive and cause destruction the middle ear, antrum, and mastoid when they reach advanced stages. The tumor's expansion of the jugular foramen on the CT scan can be a clue. CT angiography is important in making the differential diagnosis. Rarely, primary or secondary neoplasms can cause destructive lesions in the middle ear. Fibrous dysplasia is a benign but locally destructive bone tumor seen in the mastoid bone and middle ear. Malignant tumors and metastases are much less commonly observed. In a case series of 20 patients presented by Modest et al., the most common symptoms were otorrhea, subjective hearing loss, otalgia, postauricular swelling, and soft tissue swelling, respectively. In the same study, the most common finding was osteolytic lesions in the temporal bone [5]. Treatment-resistant chronic otitis with the symptoms above, unilateral disease becoming bilateral over time, or bilateral onset of the illness should bring Langerhans Cell Histiocytosis to mind in the diagnosis. A definitive diagnosis is made by detecting CD1a and S100 proteins and Birbeck granules attached to the cytoplasmic membrane in the biopsy material [4]. Chemotherapy, radiotherapy, surgery, or their combinations can be used in the treatment. In cases with multifocal involvement, the first choice is chemotherapy containing vinblastine and prednisone [6]. Multiagent chemotherapy can be considered in relapses [5]. Radiotherapy is usually given as external beam radiation in the dose range of 1000 - 1,800 cGy in locally destructive progressive diseases [4]. In local and non-large lesions, the treatment is the surgical removal of the mass, and if the surgical margin is positive, it is supported with low-dose radiotherapy [7]. The case we presented was a male patient with no complaints other than unilateral ear pain and postauricular tenderness. Although he did not have any complaints in the other ear, a lesion filling the mastoid cavity was incidentally observed in the other ear in the CT scan. Although cases of Langerhans cell histiocytosis with temporal bone involvement are common, it is rare that the patient has bilateral participation and is an adult. It should be considered in the differential diagnosis of bilateral diseases. Systemic involvement should be determined and followed up because it has been reported that systemic symptoms may begin a while after the illness that starts with temporal bone involvement [5]. In the presented case, systemic chemotherapy was not considered since the mass was limited to the temporal bone, had no involvement in another region, and had no systemic symptoms. Surgery was not considered because of extensive involvement in the temporal bone. The risk of total hearing loss and facial paralysis is high in surgery to be performed on a patient with a mass with this prevalence. At the same time, CSF leakage due to possible dural defects may be encountered. For this reason, it was decided that the patient should receive radiotherapy with the decision of the head and neck oncology council. Close follow-up of the patient after treatment is essential because the risk of relapse of the disease is high. The lesion should be followed up with 1 MRI or PET every 6 months [8]. Informed ConsentFrom the patientReferences
Presented at43.Ulusal KBB Kongresi |
|||||||
| Keywords : Temporal kemik , Langerhans hücreli histiyosiyoz , Otalji | |||||||
|