|
|||||||||||||||||||
AbstractLipoblastoma (LB) is an uncommon benign mesenchymal tumour that predominantly manifests during infancy and childhood. It is commonly seen in children under the age of three and originates from embryonic white fat cells. Although it has the potential to manifest in any part of the body, is frequently observed in the thoracoabdominal region and extremities. These lesions are exceedingly uncommon in the cervical region. The history and physical examination can narrow the potential diagnoses for the cervical masses and imaging is important for identifying the probable cause and characteristics of the mass. Knowing the surgical difficulties spesific to the head and neck region is crucial because of the anatomic relationships. In this case, the presentation, diagnosis and the treatment of an 18 months child with cervical lipoblastoma will be discussed.IntroductionLipoblastoma (LB) is an uncommon benign mesenchymal tumour that predominantly manifests in infancy and childhood [1], typically observed in children under the age of three [2]. It originates from embryonic white fat cells. [1]. These benign tumours exhibit rapid expansion and their symptoms vary based on their specific location. They have the potential to cause deformities or exert pressure on nearby structures. [3, 4]. It has the potential to manifest in any part of the body. However, it is frequently observed in the trunk and extremities. LB is extremely uncommon in the cervical region [2]. It can be categorised into two discrete types: circumscribed LB (CLB), which is enclosed within a capsule, and diffuse lipoblastomatosis (DLB). DLB is a lesion that is deeply placed and does not have clear boundaries and its growth pattern is infiltrative that could potentially affect nearby muscle components. [5, 6]. LB in the neck manifests as a fast growing mass without pain. However, in certain cases, it may exert pressure on nearby structures, leading to breathing difficulties, Horner syndrome, and hemiparesis. [7, 8]. In this case, the clinical presentation, imaging, pathological examination findings, and treatment choices of a LB that developed in the cervical region of a 1.5-year-old child will be discussed. Case ReportAn 18-month-old female applied to ENT-outpatient clinic with a six-month history of a mass on the right cervical region, which had grown by the time (Figure 1.).
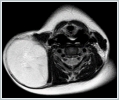
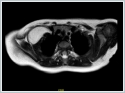
She had already underwent a fine needle aspiration biopsy at another clinic. The diagnosis was confirmed by referring it to the pathology department. The histopathological examination revealed an immature lipomatous lesion with no obvious signs of malignancy, indicating lipoblastoma. Due to the relationship of the mass with the brachial plexus and upper extremity, surgery was planned in collaboration with the orthopedics and traumatology department. The patient was given general anaesthesia, and after minimal neck extension, a transverse incision was performed (Figure 3, 4).
DiscussionLipoblastoma is an uncommon, noncancerous tumour that arises from embryonic adipose cells. Ninety percent of LB occurs under the age of three years. [9, 10]. It can be categorised into two discrete types: CLB, which is enclosed within a capsule, and diffuse lipoblastomatosis. Diffuse lipoblastomatosis is a lesion that is deeply placed and does not have clear boundaries. DLB's growth pattern is infiltrative that could potentially affect nearby muscle components [5, 6, 11]. Although they have been in the head and neck, shoulder, inguinal region, axilla, back, and abdominal cavity, these tumours typically appear in the extremities [12, 13]. A rapid growing, painless neck mass is the typical presentation of cervical lipoblastoma; but, on occasion, it can compress nearby structures and cause hemiparesis, Horner syndrome, and respiratory issues. [7, 8]. The differential diagnosis for the neck masses can be narrowed with the help of the history and examination. Additionally, imaging is crucial for identifying the features and most likely aetiology of neck masses [14]. The imaging technique that can identify these lesions the best is magnetic resonance imaging (MRI) [15]. According to a comprehensive analysis, MRI was the most commonly used method for evaluating LB, accounting for 49% of cases. This was followed by computed tomography (CT) at 36%, ultrasound (US) at 28%, X-ray at 8%, and airway endoscopy at 2%. In 11 cases (21%), preoperative biopsy was carried out in this systematic study [16]. Myxoid liposarcoma is the differential diagnosis that matters the most. Imaging does not differentiate lipoblastoma from myxoid liposarcoma. But the patient's age is crucial. Liposarcomas are incredibly uncommon in those under the age of ten. [5]. Therefore, in the case of a young child (under 2 years old), if an imaging scan shows a lesion that contains fat, it is most likely to be a lipoblastoma [17, 18]. When possible, doing a complete surgical removal is curative for these lesions [15]. Understanding the anatomical links is essential for recognising the specific surgical challenges associated with the head and neck region [15]. One case was the misidentification of a lipoblastoma as a neurofibroma, leading to the removal of the spinal accessory nerve [19]. The tumor's relationship with the brachial plexus, adjacent vessels like subclavian vessels, and mediastinum in multiple cases caused significant difficulties and challenges during the surgical removal. Sun and Hilsinger (2003) documented a case which is a lipoblastoma in the neck in close proximity to the spinal cord. In this situation, subtotal resection was chosen to avoid any potential damage to the spinal cord [20]. In the presented case, there was no injury to the adjacent anatomical structures. Postoperative evaluations indicated that the neurological functions of the right upper extremity, where the surgery was performed, and the functions of the cranial nerves were preserved. There have been no reports of metastases or malignant transformation. LB is a well-defined and localised lesion, often measuring less than 6 cm in diameter. However, there have been instances of larger lipoblastomas have been documented as in the presented case [12, 21]. ConclusionLipoblastoma should be considered as a potential diagnosis in cases of adipose tumours in children under the age of 3, and should be mentioned as a possible cause of cervical masses. It is necessary to examine the mass with preoperative radiological examinations and determine its extension areas. Surgical removal of the tumour is the preferred treatment. Due to the critical anatomical relationships, the excision of a mass in the cervical region should be performed with extreme caution to prevent long term complications. Informed ConsentFrom parentsReferences
Presented at42nd Turkish National Otorhinolaryngology and Head and Neck Surgery Congress which was held at 3-7 November 2021, Cyprus |
|||||||||||||||||||
| Keywords : Lipoblastom , boyun , benign neoplazm , infant | |||||||||||||||||||
|