|
|||||||
AbstractWe report a case of sinonasal intravascular papillary endothelial hyperplasia presenting.In this paper, IPEH in the left nasal cavity causing nasal obstruction and recurrent massive epistaxis was reported together with the clinical and radiological findings. Intravascular papillary endothelial hyperplasia (IPEH) or Masson’s tumor is a rare, abnormal thrombus formation due to non-neoplastic proliferation of the endothelium. IPEH must be kept in mind in case of massive epistaxis, and in the differential diagnosis of hemorrhagic nasal masses although it is seen very rarely in the nasal cavity. IntroductionIntravascular papillary endothelial hyperplasia (IPEH) or Masson’s tumor is a rare, abnormal thrombus formation due to non-neoplastic proliferation of the endothelium [1]. It is a benign intravascular lesion that can be mistaken for angiosarcoma both clinically and histopathologically [2-4]. IPEH is most frequently seen in the head and neck region and the extremities [1,3]. It is rarely seen in the sinonasal region [4,5]. In this paper, IPEH in the left nasal cavity causing nasal obstruction and recurrent massive epistaxis was reported together with the clinical and radiological findings. Case ReportA 58-year-old male was admitted to Ankara Numune Education and Research Hospital Otorhinolaryngology Clinic with the complaints of nasal obstruction, headache, and recurrent massive epistaxis that had been present for approximately 8 weeks. The systemic physical examination findings of the patient were normal. On nasal endoscopy, a hemorrhagic and exophytic mass containing hemorrhagic foci was seen. The mass filled the left nasal cavity completely. The patient had proptosis of the left eye. He did not have any cervical masses, and his otorhinolaryngologic examination was normal except aforementioned findings. The laboratory parameters (complete blood found and blood chemistry), and the lung X-ray of the patient were normal. The paranasal computerized tomography (CT) revealed a mass starting from left ethmoid base filling the ethmoids, and upper and middle parts of the nasal cavity. It destructed the lamina papyracea, extended into extraconal orbital fat, and neighbored medial and inferior rectus muscles. The mass also destructed the medial and posterior walls of left maxillary sinus, extended into sphenonasal recess, and obstructed the ostium of the sphenoid sinus. It also extended to left inferior orbital fissure, pterygopalatine fossa, and masticator space. The orbital magnetic resonance imaging (MRI) showed a 48 x 40 x 54 mm expansive mass in the left ethmoid region. The mass destructed lamina papyracea, extended into orbital extraconal fat, pushed medial and inferior rectus muscles laterally, and extended into the maxillary sinus and left sphenoid sinus as well as left nasal cavity, choana, and pterygopalatine fossa. The mass was heterogenous and hypointense in T1A, and heterogenous and hyperintense in T2A series, and had a heterogeous contrast enhancement after intravenous injection of the contrast material (Figure 1).
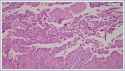
Angiography of bilateral common carotid and external carotid arteries was performed to determine the vascularity of the tumor since the patient had massive epistaxis. It showed that the mass was vascularized by left internal maxillary artery, then the vessel was embolized. Bleeding of the mass decreased after embolization, and we performed a punch biopsy. The histopathological report was intravascular papillary endothelial hyperplasia (Masson’s tumor). Surgery was planned. During surgery, the mass was removed through a lateral rhinotomy incision. It was seen that the mass filled left nasal cavity, invaded medial orbital wall, anterior wall of the sphenoid sinus, and anterior part of the pterygopalatine fossa. The mass was excised in total including the medial wall of the maxilla. The histopathological report was as follows: “On microscopy, papillary endothelial hyperplasia due to organized bleeding is seen. There are numerous recanalized papillary structures in the vessel lumen. The papillary structures are lined with endothelial cells, and they are homogenously eosinophilic. There is no significant atypia, mitosis or necrosis. These findings indicate a papillary endothelial hyperplasia (Masson’s hemangioma) originated from sinonasal sinuses (Figure 2).
DiscussionIPEH was first described by Masson in 1923 as an exophytic intravascular hemangioendothelioma [1,2,6]. The term “intravascular papillary endothelial hyperplasia” was first used by Celarkin and Enzinger in 1976 [1]. IPEH is a slow-growing benign lesion, and it most frequently appears in the head and neck region, fingers and the trunk. It is extremely rare in the nasal cavity. Its etiopathogenesis is not clear. However, hormonal and local angiogenetic factors and trauma have been accused [2]. There is no sex predilection. The mass appears as a homogenous mass on CT, while it is seen hypointense on T1, and hyperintense on T2-weighted images on MRI. Most of the mucosal IPEH cases in the head and neck region reported in English literature originated from the oral cavity. They were reported to originate from lower lip, tongue, buccal mucosa, upper lip, and mandibular vestibule [7]. We found only 7 IPEH cases in the literature that originated from the sinonasal region (Table I).
One of them originated from the nasal cavity, two from the sinonasal region, two from the maxillary sinus, and two from the ethmoids [1,3,5,7-10]. In our case, the mass was quite large, and it filled left nasal cavity, ethmoids, and maxillary sinus, and extended into the orbita. On histopathology, IPEH has a characteristic exuberant endothelial proliferation within the lumen of medium –sized veins. The lesion is well-circumscribed, intraluminar, has a papillary formation related to thrombotic material, fibrohyalinized stuck of the papillae, possibly hyperchromatic endothelial cells, uncommon piling up of endothelium, obscure cellular pleomorphism, rare mitotic activity, and rare foci of necrosis [7]. In our case, histopathological examination showed numerous recanalized papillary structures in the vessel lumen. The papillary structures were lined with endothelial cells, and they were homogenously eosinophilic. There was no significant atypia, mitosis or necrosis. The treatment of IPEH is surgical. The aim of surgery is total removal of the mass, since partial removal inevitably results in recurrence. In our case, we used a left lateral rhinotomy approach, and totally removed the mass filling left nasal cavity, invading medial orbital wall, anterior wall of the sphenoid sinus, and anterior part of the pterygopalatine fossa, and we included the medial wall of the maxilla in the specimen. IPEH can be confused with angiosarcoma both clinically and histopathologically. Endothelial proliferation limited in the vessel lumen, few or no mitoses, absence of solid regions or anaplasia, and little or no necrosis support IPEH against angiosarcoma [1]. Some cases in the literature were mistaken for angiosarcoma, and the patients had extensive surgery and radiotherapy [5]. Therefore, IPEH and angiosarkoma must be differentiated histopathologically to avoid aggressive or inappropriate treatment. In conclusion, IPEH must be kept in mind in case of massive epistaxis, and in the differential diagnosis of hemorrhagic nasal masses although it is seen very rarely in the nasal cavity. Radiologic imaging of the lesion is important; however histopathological examination is needed for the definitive diagnosis. Its treatment is total surgical excision. References
|
|||||||
| Keywords : Masson’s tümör , Sinonasal , Burun kanaması | |||||||
|