|
|||||||||||
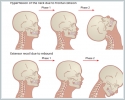
AbstractWhiplash is an acceleration-deceleration mechanism of energy transfer to the neck. Whiplash trauma is an injury of the cervical spine and soft tissue that occurs after sudden extension and flexion of the neck. As a general term for a syndrome, Whiplash syndrome can be defined as comprehended symptoms such as vertigo and disequilibrium, nausea and vomiting, neck pain and stiffness, tinnitus and hypoacousia, etc. following a traffic accident, especially rear-end collisions. We present a case report of a 44-year-old male patient who complained of vertigo after a car accident. His head was suddenly thrown backward and forwards during the collision of another vehicle to the back of his car while he was driving with his seat belt fastened. The patient suffered from the symptoms of vertigo, disequilibrium, nausea, and vomiting a few hours after the accident. No hearing loss, aural fullness, or tinnitus. On videonystagmography, the patient had mild left-beating spontaneous nystagmus, caloric test results showed unilateral weakness in the right ear. Considering the clinical findings and history, the patient was diagnosed with vertigo and whiplash-associated disorder. We present this case report to discuss the clinical picture, diagnosis, and management of a patient who had vertigo following whiplash trauma.IntroductionWhiplash injury is the trauma of cervical spine that occurs due to a sudden back and forth movement of the head during an in-vehicle traffic accident, particularly when the seat belt is fastened (Figure 1). Persistent headache, neck pain, vertigo, disequilibrium, nausea, and vomiting may be seen in 15-20% of cases after whiplash trauma, and the presentation characterized by those symptoms is called “whiplash syndrome” [1-4]. Deterioration of neural transmission between the cervical proprioceptive system and the central vestibular system has been suggested as the cause of disequilibrium and vertigo. The aim of this case report is to discuss the clinical picture, diagnosis and management of a patient who had vertigo following whiplash trauma.
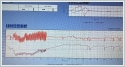
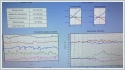
Case ReportA 44-year-old male patient was admitted to our clinic with vertigo that started after an in-vehicle traffic accident. Vertigo had been continuing for five days. His head was suddenly thrown backward and forwards during the collision of another vehicle to the back of his car while he was driving with his seat belt fastened. The patient had vertigo, disequilibrium, nausea, and vomiting a few hours after the accident. He did not have neck pain or headache. He applied to the physician and was prescribed betahistine dichloride and dimenhydrinate. The patient’s complaints continued, and he applied to the emergency department. His electrocardiogram and cerebral magnetic resonance imaging (MRI) were normal, he was prescribed symptomatic medications. The patient was admitted to our clinic five days after the accident with the same complaints. The patient did not complain of hearing loss, aural fullness or tinnitus. The patient did not have any chronic disorders or use any regular medications. The otoscopic examination, tympanogram, and pure tone audiogram were normal (Figure 2). Dix-Hallpike test, supine roll test, Romberg, and skew tests were negative, and the video head impulse test was normal (Figure 3). On videonystagmography (VNG), the patient had mild left-beating spontaneous nystagmus, caloric test results showed unilateral weakness in the right ear (Figure 4, 5). Temporal bone computed tomography, cerebral magnetic resonance imaging, and Doppler ultrasonography of vertebral arteries (USG) were reported as normal.
Considering the clinical findings and history, the patient was diagnosed with vertigo and whiplash-associated disorder after whiplash trauma. Single-dose intravenous 1 mg/kg methylprednisolone was administered at the time of admission, and betahistine dichloride 48 mg/day was prescribed as the symptomatic treatment. The patient’s complaints disappeared within two months of follow-up. Informed Consent: Informed consent was obtained from the patient involved in this study. DiscussionWhiplash is an acceleration-deceleration mechanism of energy transfer to the neck. Whiplash trauma is an injury to the cervical spine and soft tissue. The name of “Whiplash trauma” was first used in a symposium about traffic accidents in San Francisco by Crowe in 1928. It occurs during rear-end car accidents, particularly when the seat belt is on, due to rapid and forceful back-and-forth movement of the head forcing the neck joints to over flexion and overextension, beyond the normal range of motion [1-4]. According to the analysis of The Quebec Task Force, neck pain and limitation of the movement were deemed necessary after whiplash injury for the diagnosis of whiplash syndrome [2]. It has been classified in the category of whiplash-associated disorders about the post-traumatic symptoms. In most cases, balance problems or vertigo may be evident in the acute or late periods after the injury. Whiplash-associated disorder (WAD) is a term for a soft tissue injury of the neck with symptoms such as neck pain and stiffness, headaches, dizziness, visual symptoms, cognitive and psychiatric disorders, paresthesias, and weakness. Many patients after whiplash injury recover fast, but, between 4 and 42 % of patients can suffer from symptoms several years later the trauma. Dizziness can be seen in 70% of patients with whiplash injuries [2,3]. Literature data indicates that post-traumatic balance and hearing problems may occur in 5-50% of the individuals who had whiplash trauma [1]. Although the pathophysiologic mechanisms of imbalance and vertigo have not been clearly defined, vertigo and disequilibrium occur mainly due to damage to the neck joints, cervical vasculature, neck muscles, or neck ligaments after trauma, affecting the cervicospinal proprioceptive signal pathway which is associated with the central vestibular system [5]. Not only a direct effect of the trauma in the inner ear but also damage to vessels supplying the inner ear have also been suggested for the reason of vertigo [4].Ischemia due to vertebral artery compression, hemorrhage, concussion of the labyrinth, or acoustic trauma due to noise during collision has also been accused as possible causes [3,4]. In Ommaya’s hypothesis, an abnormal stretching of the cerebrum, and sudden transient increase of the pressure cerebrospinal fluid that cause neuropsychological symptoms after whiplash trauma provoked a commotio cerebri with potential injuries to the temporal cortex, amygdala, hippocampus, medial temporal cortex, corpora mammillaria, medial thalamus, basal nuclei, prefrontal cortex, and retrosplenial cingulate cortex [2,6]. Differential diagnosis of vertigo due to whiplash trauma should be considered with clinical evaluation of peripheral labyrinthine pathways and vestibuloocular reflex arc by using clinical vestibular tests, videonystagmography, and caloric tests [2,7]. The meta-analysis of Faveretto et al. including 700 cases reported the most frequent symptoms as disequilibrium, positional symptoms, and neck pain. Impaired vestibuloocular reflex, spontaneous nystagmus, and bilateral vestibular hypofunction were frequently observed on VNG. The authors suggested that VNG and caloric tests were helpful in the diagnosis [4]. Endo et al. detected unilateral vertebral artery occlusion on neck MRI angiography and unilateral slow vertebral artery flow on Doppler USG in a patient who had headache, neck pain and dizziness that were present for months after whiplash trauma [7]. BPPV may also be seen after whiplash trauma, and it should be included in the differential diagnosis of vertigo, particularly if the patient has a history of head trauma [3,8]. In the treatment of vertigo following Whiplash trauma, symptomatic therapy involves vestibular suppressors and antiemetic drugs are suggested. Antihistaminic drugs such as dimenhydrinate, flunarizine, cinnarizine, hydroxyzine, and betahistine can be used immediately and continued for a few days. Benzodiazepines can also be used for inhibitory effects on vestibulocerebellar pathways and vestibular nuclei by GABAergic activation. Benzodiazepines should be carefully administered in elderly patients to avoid respiratory inhibitor effects [2]. ConclusionIn cases applying vertigo, disequilibrium, and neck pain after traffic accidents, whiplash-associated disorders, and whiplash trauma should be kept in mind, and the diagnosis should be supported by VNG and caloric testing. Vertigo can be the only symptom associated with whiplash trauma. While appropriate treatment is used for vestibular rehabilitation, symptoms can release within the follow-up. In addition, vertebral artery Doppler USG should be used for the excluding the vertebral artery occlusion. References
|
|||||||||||
| Keywords : vertigo , dengesizlik , whiplash sendromu , whiplash travması , trafik kazası | |||||||||||
|