|
|||||||
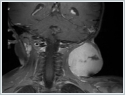
AbstractInflammatory myofibroblastic tumor is a rare benign tumor that forms infiltration which is composed of myofibroblastic spindle cells. It is usually seen in the field of mesenchymal region and rarely head and neck region. A child was hospitalized with acute lymphadenitis that was presented with swelling in the left side of neck and fever. Despite of medical antibiotics therapy, the ultrasound imaging of mass was seem to be progressed and magnetic resonance imaging (MRI) revealed a hyper vascular mass. As rapid progression in mass size was seen, incisional biopsy was performed and pathology was interpreted as inflammatory myofibroblastic tumor. Total excision of the mass in the neck was performed under general anesthesia in this rare phenomenon. There were no complications after the operation. Inflammatory myofibroblastic tumor diagnosed patients whom we operated are presented with clinical findings and treatment comparing with literature data.IntroductionInflammatory myofibroblastic tumor (IMT) is a rare benign tumor composed of myofibroblastic spindle cells that shows infiltration. Generally it is seen in the mesenchymal areas and rarely in the head and neck region. Different clinical findings can be seen according to the localization [1]. Few cases have been reported that detected IMT over the course of the disease. Therefore, it is difficult to diagnose. In this study, it is aimed to discuss clinical findings, imaging methods and treatment options of this rare case. Case ReportA 2-year-old case applied with a fever of 38.5 degrees and swelling on the left side of neck despite of ongoing 3 days of amoxicillin clavulonic acid therapy and hospitalized with acute lymphadenitis diagnosis. The treatment was consisted with intravenous ampicillin sulbactam 150 mg / kg / day in 4 doses. There was no significant result except high erythrocyte sedimentation rate (69 millimeters (mm) / hour) in laboratory tests. Ultrasound imaging of revealed suspicion of 23x21 mm malignant lympadenopathy and fine needle aspiration (FNA) was performed. Pathology results did not give any diagnosis so MRI was performed the size of the mass showed rapid progression. MRI revealed a solid mass of 46x60 mm in size and incisional biopsy was performed.
Pathologic diagnosis of the biopsy was evaluated as inflammatory myofibroblastic tumor. After the biopsy the size of the mass showed rapid progression. Total mass excision was planned under general anesthesia. During the operation it was seen that the mass was fragile and there was a partial invasion to the sternocleidomastoid muscle. However, the jugular vein and carotid artery invasion was not observed. By dissection from the surrounding tissue, total excision of the mass was performed which was about 8x6 centimeters.
Surgical site was closed in accordance with the anatomic plan and a hemovac drain was placed. Post-operative first day 75 cubic centimeter (cc) hemorrhagic fluids were drained and 40 cc on the second day. As no fluid came from drain, the drain was removed on the third day. At the end of the first week, the suture was taken out and discharged as no problem was noted. The patients were followed up monthly for six months. After 12 months follow up, there is no clinically significant problem. DiscussionIMT is a tumor that is consisted from myofibroblastic cells with rare mitosis [1]. IMT was defined first by Pettinato with 20 pseudotumor cases [2]. It was first identified in the lung and after that larynx, breast, bladder, central nervous system, pancreas, orbital, mesenteric, prostate, neck, salivary glands, spleen, skin and rete testis involvements have been reported. As usually it occurs in children and young adults it may be seen at any age [3]. Hematological tests often show an increase in erythrocyte sedimentation rate. High erythrocyte sedimentation rate (69 mm / h) was observed in this case as well. It is difficult to diagnose because of the complex pathological structure. So it is evaluated with radiological imaging and clinical examination. IMT usually appears as a homogeneous or heterogeneous soft tissue mass extending into adjacent tissues on radiological imaging’s [4]. In our case the homogeneous contrast holding hyper vascular solid mass was observed as pushing the sternocleidomastoid (SCM) muscle. The most effective treatment is surgical excision as IMT is not an aggressive tumor [5]. Total excision of IMT was performed by partially excising sternal branch of SCM muscle in this case. Some studies indicate that high doses of steroids and radiotherapy treatments are important treatment options for IMT on the larynx. Suh et al suggest that steroid therapy is a good option for the treatment of IMT on steroid larynx [6]. However, there are no studies in the literature indicating the success for IMT in the neck. In this case, as stated in the literature, total excision of the mass was performed by preserving the vital organs. However, if the mass can not be fully excused, recurrence can be observed. Therefore, postoperative follow-up is important [7.8]. Within six months after the operation monthly follow up was performed and after one year there was no recurrence finding. As it is hard to diagnosis and seen with a low incidence in head and neck region, local resection is an effective treatment option for IMT. Careful postoperative follow-up should be performed in terms of local recurrence. References
Presented at8. Cerrahi Araştırma Kongresi, 12-14 Kasım 2015 Konya |
|||||||
| Keywords : Boyun , inflamatuar , tümör | |||||||
|