|
|||||
AbstractThe nasal cavity is an uncommon site for a cavernous hemangioma. Cavernous hemangiomas of middle turbinates are very rare. Pneumatization of the middle turbinate, also known as concha bullosa, is a common anatomical variation of the sinonasal region. We describe a case of a cavernous hemangioma of the nasal cavity with a prediagnosis of concha bullosa of the middle turbinate according to computed tomography (CT) findings. Paranasal CT studies showed pneumatization of the middle concha. Given the prediagnosis, partial resection of the middle turbinate was performed instead of complete resection. The patient was followed up for 2 years. There was no enlargement of the middle turbinate after surgery. Three interesting aspects of the present case were the rarity of the site of the hemangioma, nonspecific symptoms, and radiological findings, which pointed to a different pathology i.e., concha bullosa. To our knowledge, this is the first reported case in the English literature of cavernous hemangioma with a prediagnosis of concha bullosa.IntroductionHemangiomas account for 20% of all benign neoplasms of the nasal cavity [1]. Cavernous hemangiomas of middle turbinates are very rare. In contrast, pneumatization of the middle turbinate, also known as concha bullosa, is a common anatomical variation of the sinonasal region. The characteristic computed tomography (CT) finding of a cavernous hemangioma is a large, inhomogeneous mass [2]. We describe a case of cavernous hemangioma with a prediagnosis of concha bullosa of the middle turbinate according to CT findings. Informed consent was obtained from the patient. Case ReportAn 80-y-old female presented with an approximately 1-year history of nasal obstruction. The patient had no history of epistaxis or trauma. A rhinoscopic examination revealed right-sided hypertrophy of the middle turbinate, with left-sided septal deviation. The middle turbinate was covered with normal mucosa. Computed tomography (CT) (SOMOTOM; Siemens, Earangen, Germany) showed left septal deviation and extensive pneumatization (concha bullosa) of the right middle turbinate, with chronic inflammation of the maxillary (bilateral), ethmoid (left), and frontal (left) sinuses (Figure 1).
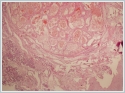
The patient underwent surgery under general anesthesia. After removing the lateral part of the concha, submucosal resection of the deviated septum and endoscopic sinus surgery for the affected sinuses were performed. There was no excessive bleeding during surgery, and a carboxymethyl chitosan-based hemostatic intranasal splint (PosiSep X; Hemostasis.LLC, St.Poul, USA) was sufficient for control of bleeding. A histopathological examination showed that the tumor was composed of bony trabeculae and vascular channels consistent with a cavernous hemangioma (Figure 2).
DiscussionHemangiomas are benign vascular tumors of the skin, mucosa, muscles, glands, and bones [1]. These are divided into the capillary, mixed and cavernous types [3–5]. Although these tumors are common lesions of the head and neck, they rarely occur in the nasal cavity and paranasal sinuses [1]. Cavernous hemangioma of the nasal cavity and paranasal sinuses was described as arising from the inferior turbinate, vomer, lamina perpendicularis ossi ethmoidalis, and sinus maxillaris [1,3,5]. To the best of our knowledge, only three cases of cavernous hemangioma of the middle turbinate have been reported in the literature [6–8]. The pathogenesis of intraosseous hemangiomas is not clear. Local trauma may be a cause because many patients with intraosseous hemangiomas have had a history of local trauma [9]. However, our patient had no history of either facial trauma or nasal surgery. The nonspecific clinical presentation of hemangiomas makes it difficult to differentiate them from other nasal tumors, as was the case with our patient. Kim et al. reported a case of a cavernous hemangioma that arose from the middle turbinate and was preoperatively misdiagnosed as a polyp [1]. The most common symptom of intraosseous hemangiomas is not epistaxis but rather nasal obstruction due to a mass, as in our case [1]. Per the literature, a radiographic examination is useful for making a preoperative diagnosis when calcifications and bone destruction are adjacent to a hemangioma [3,10]. Bony changes in cavernous hemangiomas include remodeling or erosion with the smooth, nonaggressive cortical breakthrough. Kim et al. reported that four of six cavernous hemangiomas showed benign-appearing smooth bony remodelings, such as nasal septal deviation, widening of the ethmoid sinus and infundibulum, and either uncinated process or middle turbinate remodeling [9]. Computed tomography imaging of our case did not reveal any characteristic findings of a hemangioma. This can be related to the benign-appearing smooth bony remodeling effect of the cavernous hemangioma, as Kim et al. stated. Paranasal sinus CT imaging of our case found pneumatization of the right middle concha with septal deviation, chronic inflammation of the maxillary [bilateral], ethmoid [left], and the frontal [left] sinuses. In the absence of a malignant transformation risk, a trans-nasal endoscopic approach has been recommended as the surgical technique for the complete removal of a hemangioma, either with or without embolization [3]. Because our first diagnosis was a concha bullosa, partial resection of the middle turbinate was performed instead of complete resection. Follow-up is necessary to identify recurrences, even in cases of complete resection. In the present case, the patient was followed up for two years, with the nasal obstruction and headaches resolved after surgery and no recurrence of a similar lesion. Follow-up examinations are continuing. Conclusion Surgeons should consider the possibility of a cavernous hemangioma when performing middle turbinate surgery. Cavernous hemangiomas can be in the form of isolated lesions or can be found with other lesions as our case. The nasal endoscopic technique is reliable for turbinate surgery with adequate exposure and visualization of the lesion. References
Presented atThis study was presented as poster presentation at the 4th Congress of European ORL-HNS Barcelona, 2017. |
|||||
| Keywords : kavernöz hemanjiom , orta konka , konka bulloza | |||||
|